Thyroxine: A Deep Dive into Its Journey, Properties, and Future
Historical Development
Discovery stories often carry a weight of trial and error, and that fits the timeline for thyroxine. Late in the 19th century, scientists struggled to grasp why the thyroid gland mattered. After early work with sheep thyroids and some gut-level intuition, the search for the “active principle” kept going. By 1914, Edward Calvin Kendall isolated thyroxine in pure form. This wasn’t just another chemical sitting in a lab; doctors suddenly saw hope for treating thyroid disorders, a constant mystery for medics baffled by weight changes, mood swings, and unexplainable fatigue. The move from crude animal extracts to pure, synthesized crystalline thyroxine meant that treatment left behind inconsistent batches and primitive guesses. Each decade since has built on this lift—better purity, more precise dosages, and less reliance on livestock. Lab staff still remember pouring over early greying journals, seeing how far the industry has moved from animal-stuffed capsules to controlled, fine powders on stainless steel trays.
Product Overview
Thyroxine, also known as T4, ranks among the most essential hormones humans rely on. It goes by a range of names in hospital pharmacies and chemical suppliers—levothyroxine, L-thyroxine, and even just “T4” in shorthand. Doctors reach for it to treat hypothyroidism, and it slips into almost every endocrinologist’s toolbox for balancing thyroid function. Veterinary circles also keep it on hand, given that household pets and livestock can face thyroid troubles much like people do. Tablets, injectables, and powders crisscross the broad supply chain. What stands out about thyroxine compared to other replacement hormones is its sheer predictability in effect, as long as manufacturing holds up its end.
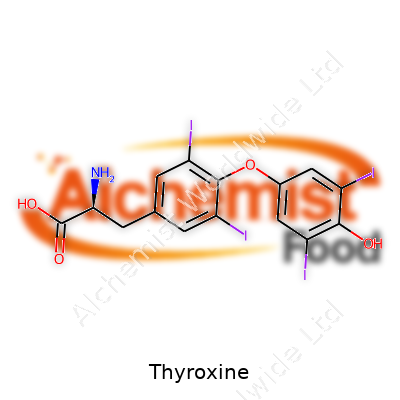
Physical & Chemical Properties
In pure form, thyroxine comes as an off-white to pale yellow crystalline powder. It holds up well to air but doesn’t fare so great in strong sunlight. Water barely moves it, but it dissolves smoothly in alkaline solutions and glacial acetic acid. People working in chem labs recall handling it with the respect given to faint, dusty powders that pack a punch in microgram doses. Its molecular formula, C15H11INO4, includes four iodine atoms—a nod to its roots in the iodine-rich thyroid gland. High melting point, close to 235°C. Molecular weight lands at about 776.87 g/mol, and lab techs note its stubborn stability on the shelf, as long as light and moisture stay out of the equation.
Technical Specifications & Labeling
Suppliers print specs on thyroxine containers that demand close attention: content often 98-102% by HPLC, usually with detailed reference to United States Pharmacopeia or European Pharmacopeia monographs. Labels lay out recommended storage under 25°C, away from light, sealed tight. Pharmacies package tablets in blister packs or amber bottles, calling out lot numbers and stamped expiry dates within two to three years of manufacture. Regulatory strings demand clear warnings about dosing, potential interactions, and contraindications—typical of any potent hormonal product. Because microgram-level overdoses spark big problems, plenty of fuss goes into pill size, scoring, imprint coding, and container warnings—a complexity that limits errors in busy hospital wards.
Preparation Method
Modern production leans hard on chemical synthesis. The classic route starts with derivatized tyrosine, which meets iodine sources in controlled reactions. Industrial labs often prefer routes that allow for chirality—the body only responds to the L-form, so careful construction avoids unwanted D-thyroxine contamination. High-vacuum distillation, chromatography, and crystallization come into play to achieve drug-grade purity. In research settings, older extraction methods from porcine or bovine glands still see use, often for assay calibration or comparative studies. Personnel in these plants sweat every step, since one slip in system cleanliness or reaction conditions ruins whole batches, and quality checks catch even the smallest off-color batch before release.
Chemical Reactions & Modifications
Thyroxine stands open to a few key modifications in the lab. Iodine atoms can be swapped or removed—scientists use this for tracking isotope-labeled derivatives in studies, or in creating analogs with altered half-lives. Reduction reactions slice off an iodine atom, making triiodothyronine (T3), which actually drives many of thyroxine’s effects inside the body. Acidic conditions can cleave certain bonds, though the hormone resists breakdown under physiologic pH. Biotech researchers also tinker by attaching carbohydrate side chains, chasing experimental compounds for targeted tissue delivery or slow-release action. Plenty of grad students spend evenings tracking fluorescence-labeled forms through cell cultures, all in hopes of discovering a quicker diagnostic test.
Synonyms & Product Names
Thyroxine answers to plenty of names across the world: levothyroxine sodium in North America, L-thyroxine in scientific circles, and Euthyrox, Synthroid, Levothroid, Levoxyl, Unithroid among branded options at the pharmacy. The CAS number, 51-48-9, fixes its identity for regulatory and shipping paperwork. To avoid mix-ups with T3, staff double-check packaging, often with both INN (International Nonproprietary Name) and the local trade name printed large at every step, especially as lookalike generic names swirl through patient prescriptions and global shipments.
Safety & Operational Standards
Strict safety guidelines run through any lab or plant handling thyroxine. Microgram-level exposure tosses thyroid balance off in staff, so clean benches, gloves, and dust masks make up daily ritual. Any weighing needs analytical balances with draft shields; spillage triggers immediate cleanup with sealed bags and wipe-downs, since the dust’s invisibility adds a sneaky layer of danger. Industry hazard sheets rate levothyroxine as potentially toxic if inhaled in powder form. Environmental protocols prevent hormone-laden wastewater from entering municipal drains, since even trace hormone levels disrupt aquatic wildlife. Supervisors check records on personal protective equipment use, and regular staff health checks catch unexpected overexposure.
Application Area
Doctors across the spectrum rely on thyroxine, mostly for treating underactive thyroid—whether from autoimmune destruction, after surgery, or in newborns with congenital hypothyroidism. Patients need dosing adjusted to age, pregnancy status, and other meds, as absorption swings around food, vitamins, and calcium. Outside of patient care, scientists watch for thyroxine disruptions as markers of environmental toxin exposure in wildlife and humans. It also enters the mix when managing thyroid cancer, helping suppress tumor regrowth. Livestock and pets gain from tablets and premixes in animal health, with busy dairy operations often tracking herd thyroid levels nearly as much as milking schedules. Basic and clinical researchers test synthetic variants in metabolic disease models to probe everything from cholesterol handling to brain growth—its reach seems to keep expanding with each new publication.
Research & Development
This field never runs out of new angles. Early R&D tracked better synthetic routes to pure L-thyroxine, then shifted to formulations that reduce day-to-day swings in patient levels. Ongoing work extends to slow-release tablets and liquid solutions with improved taste for infants. Scientists keep one eye on transporter proteins that ferry thyroxine into cells, searching for treatments that can bypass defects in those pathways. Even in 2024, new studies pop up about gene variants that tweak dosing needs, forcing pharmaceutical companies to rethink old standards. Some tech firms chase digital pills and stick-on monitors that automate dosing or warn about missed medication days—a push towards tech-enabled, ultra-individualized thyroid care.
Toxicity Research
Safety margins for thyroxine look thin; it’s one of those drugs where too much acts almost as badly as too little. Poison control centers report heart palpitations, anxiety, heat intolerance, and weight loss after accidental ingestion or too-high dosing. Chronic excess tips into osteoporosis and muscle loss, not just arrhythmias. Toxicity studies fed into product labeling: older adults and newborns need less; careless dosing in kids costs neurodevelopmental ground. Animal trials flag reproductive and neurologic risks with gross overdose. Field researchers sometimes track urban wastewater for hormone residues, connecting excess levels to fish with altered reproductive skis. That evidence pushed regulators to update disposal methods and reinforce handling protocols in hospitals and pharmacies.
Future Prospects
The next decade holds big shifts for thyroxine. Innovations eye formulations that dodge the wild swings in blood levels some patients endure. Gene-guided dosing creeps closer, raising hopes for simple blood tests that fine-tune starting doses before symptoms ever flare up. Better home testing technology inches from dream to mainstream, promising people real-time insight into their own thyroid status, so missed doses don’t go unnoticed for weeks. Researchers experiment with modified thyroxine, built to reach trouble spots in the brain or heart, offering new hope for stubborn depression or congestive heart failure tied to thyroid function. Pharmaceutical firms push green chemistry production routes, aiming to slice energy costs, waste streams, and environmental risks. Education also gets a boost, with expanded pharmacist roles and digital tools cutting medication errors. The story of thyroxine stands far from finished—every batch pressed, every lab trial set up speaks to a future where hormones and tech work together for faster, safer, and more precise care.
What is Thyroxine used for?
Why Doctors Prescribe Thyroxine
Over the years of seeing friends or relatives struggle with sluggish moods, stubborn weight gain, and mental fog, I keep coming back to stories about low thyroid function, or hypothyroidism. For lots of folks, the answer from the doctor turns out to be a daily tablet called thyroxine. It’s a synthetic form of a natural hormone, and it’s on pharmacy shelves across the country. Yet, outside of doctor’s offices, people still scratch their heads about what it actually does.
At its core, thyroxine replaces or supplements a hormone your thyroid gland should be making. Missing this hormone leads to all kinds of trouble — think slow metabolism, chilliness even when the sun is out, low mood hovering like a gray cloud, and even hair thinning. Studies from places like the Mayo Clinic show that over 10 million people in the U.S. are on thyroid hormone therapy, most of them taking thyroxine. Thanks to years of medical research, most prescribers can pinpoint the right dose for a patient just from a morning blood test and some conversation about how life’s going.
Why Thyroxine Matters
This is more than just a pill for “feeling better.” Untreated hypothyroidism leads to rising cholesterol, aching joints, infertility, and life-threatening situations like myxedema coma. My own relative had months of strange exhaustion before simple blood work revealed the culprit. After starting thyroxine, it was like watching color return to a faded photograph. Half a tablet a day kept her working, walking, and enjoying food again.
Pregnant women need their thyroid hormones more than ever. Medical experts underline that low levels in mothers can cause problems with the baby’s brain and nerves. The American Thyroid Association points to thyroxine’s safety in pregnancy, provided the right levels are checked along the way. That kind of reassurance matters to anxious new parents who only want the healthiest start for their kids.
Challenges With Thyroxine
It’s not all smooth sailing. Missing doses, taking supplements that mess with absorption, or buying knockoff pills online can all spell trouble. In my work with patients, I’ve seen the frustration when energy dips return because the thyroid wasn’t getting the help it needed. Experts at the Endocrine Society report that food, calcium, and iron supplements can block how well thyroxine works. Even different brands might act a little different in your body, which sometimes means labs need rechecking after a switch.
Solutions and Smarter Use
Reliable thyroid care means honest communication. People taking thyroxine should ask questions at the pharmacy, be upfront about pesky symptoms, and speak up about pills from new suppliers. Doctors can use routine blood tests — checking TSH and free T4 — to keep things in balance. Pharmacies should be letting patients know about drug or supplement interactions. For anyone unsure, groups like the American Thyroid Association offer down-to-earth resources and even helplines.
Knowledge about thyroxine isn’t just medical trivia. It’s about helping people get back to themselves after weeks or months of not feeling right. As more patients seek healthcare online and medication by mail, clear and science-backed advice keeps thyroid treatment running safely and smoothly.
How should I take Thyroxine?
Thyroxine and Everyday Life
Living with thyroid issues makes daily routines more deliberate, especially around medication. Thyroxine’s job is to replace or supplement your body’s natural thyroid hormone, and those tiny pills come with some big instructions. After more than a decade managing hypothyroidism, it becomes clear that timing, food, and patience play a huge role in whether those tablets do their job.
The Best Way to Take Thyroxine
Doctors and pharmacists agree on the basics: take thyroxine in the morning, on an empty stomach, with just water. Even small changes can impact how well your body absorbs it. Research published in the journal Thyroid points out that food, coffee, and some medicines can reduce how much of the hormone your gut takes in by half.
Experience backs this up. A coffee right after swallowing the pill sometimes left my blood tests looking off — fatigue, weight gain, and brain fog lingered. Skipping breakfast for at least half an hour afterward brought noticeable improvements. It's tough at first, but that consistent window makes all the difference.
Common Mistakes People Make
Plenty of folks grab their tablet with breakfast, or forget and double up. Sometimes it’s easy to brush off advice and just fit the pill in where it seems convenient, but small things chip away at its effectiveness. Calcium from milk or breakfast cereals and iron supplements block absorption. Antacids and even some multivitamins cause trouble, too.
Personal experience taught me to shift any calcium to lunchtime and keep iron at dinner. It’s a pain to stagger everything, but blood tests show better hormone levels, which means fewer symptoms. For people balancing multiple medications, a pharmacist can map out a safe schedule.
Checking In With Your Healthcare Team
Thyroid hormone needs shift over time, because bodies and lifestyles change. Stress, diet changes, pregnancy, aging — all these throw curveballs. Regular blood tests give insight into whether the dose still fits.
Taking thyroxine at a sporadic time or skipping days throws off lab results. Returning to the same time and being strict about fasting helps doctors read your results with confidence and adjust your dose if needed.
Improving Daily Thyroxine Habits
People sometimes try apps, alarms, or tying the routine to another consistent habit, like brushing teeth. These small tricks ease the load and push the brain to remember. For those who can't make morning work, some endocrinologists say bedtime works — just keep it at least two hours after the last meal. A study in the Archives of Internal Medicine claims it works just as well.
Sticking with the same brand also helps, as generic tablets can vary just enough to cause a dip or spike in hormone levels. Noticing changes after switching brands, I called the pharmacy and asked to return to the same label; symptoms mellowed out, and things felt stable again.
Building a Strong Routine
Taking thyroxine isn’t just about swallowing a pill. It means setting up guardrails — avoiding food for at least 30 minutes, watching for hidden blockers, and communicating openly with your healthcare team. These choices impact energy, mood, weight, and even heart health. It’s about making an invisible hormone visible in daily decisions, for a more predictable, comfortable life.
What are the possible side effects of Thyroxine?
Real Experience with Thyroxine
Years ago, after being diagnosed with hypothyroidism, my doctor handed me a prescription for thyroxine. I hoped it would bring back the energy and sharp thinking I had lost. Thyroxine works—there’s no denying that. It supplies a hormone that many of our bodies just don’t make enough of anymore. Many people step into this same spot, expecting only the benefits. But even something this necessary can kick up a few side effects.
Why Side Effects Appear
Thyroid hormones drive so many basic functions—think metabolism, energy, body temperature, and mood. Tinkering with hormones means rippling effects across these functions. Sometimes the dose isn’t a perfect fit. People whose doses run a little high might start feeling jumpy, sleepless, or even anxious. Others get muscle weakness or unexpected weight loss. Some of my friends taking it have talked about sweating more, or feeling their hearts race at rest.
Common Side Effects I Have Seen or Heard
Heart racing stands out. Supplying too much thyroxine can push the heart into overdrive. I remember a time when I felt my heart pounding in my chest after my dose was increased. Plenty of users complain about feeling shaky or nervous—not at all the calm people expect after starting thyroid therapy. Headaches show up for some. Changes in menstrual flow appear too. My neighbor started thyroxine and her periods became more frequent for a few months before settling down.
Weight loss sounds great to most people, but on thyroxine, it can signal trouble. Muscles can feel weaker, and stamina drops. Insomnia creeps in. Some friends lost hair for a few months on the new medicine. These aren’t rare stories. Published data from large studies show that too much thyroid hormone sooner or later starts to act out in these ways.
Long-Term Concerns and Careful Monitoring
Taking thyroxine over months or years without regular check-ups opens the door to bigger issues. Research from reputable sources like the Mayo Clinic and British Thyroid Association highlights bone loss as a real risk when doses run high for too long. In older people, going long stretches with excess thyroxine can set up atrial fibrillation, making the heart beat unevenly. Not everyone talks about these problems at first, but careful doctors watch out for them.
Children and the elderly need special care with this drug. Children’s growth and brain development depend on the right amount. Too much, even for a short stretch, might throw off their bone growth or cause hyperactive symptoms. In older folks, fragile bones become a real problem if they absorb too much thyroxine month after month.
How to Lower the Risk
Getting the dose just right makes all the difference. Blood tests like TSH, T4, and sometimes T3 steer the dose toward the sweet spot. For most people, routine checks—every few months at first, then every year—keep things in line. If any of those common side effects from above turn up, it’s worth checking levels quickly. Changing pharmacies or brands can matter too, since not all generic versions act the same.
Talking openly with a doctor and reporting symptoms quickly keeps the risks low. Keeping a written symptom log helped me catch a dose problem before it got serious. Thyroxine remains a crucial—and safe—medicine for most people with thyroid disorders. Regular contact with a skilled healthcare provider and attention to new symptoms protect long-term health.
Can I take Thyroxine with other medications?
Thyroxine and the Pill Routine
Prescription bottles crowd the shelves and each one comes with its own label of dos and don’ts. Thyroxine, the trusted backup for an underactive thyroid, comes with rules that can trip up even experienced patients. Sticking to the correct approach matters. Absorption gets complicated when other drugs elbow their way into the mix. That lesson hit home for my neighbor, Rita, who wondered why her thyroid numbers never budged. Her daily cup of coffee, rushed in right after her pill, didn’t do her any favors.
Timing Comes Into Play
Thyroxine doesn’t like to share the stage. Taking it on an empty stomach, then waiting at least 30 minutes before food or coffee, earns the best results. Skimp on this window, and absorption drops. It doesn’t stop with coffee or toast—supplements like calcium or iron can grab thyroxine, trapping it in the gut before it gets a chance to work. Studies back this up. A paper in the Journal of Clinical Endocrinology and Metabolism shows that calcium or iron, even several hours apart, can mess with hormone levels. Lining up the day’s pills in a row may seem efficient, but thyroxine prefers an early solo act.
Common Medication Roadblocks
Many families keep antacids or supplements close at hand. These blockades rarely come up in conversation during short doctor visits. Antacids, especially those with aluminum or magnesium, hold onto thyroxine molecules, so less of the hormone gets to where it needs to go. Heartburn remedies like omeprazole change gut pH, shifting absorption further. Blood thinners, diabetes medicines, and certain antidepressants have their own quirks. The American Thyroid Association keeps reminders front and center: always update your doctor about every pill you take, including all those “just vitamins.”
Why This Matters for Daily Life
Missing the mark with thyroid medication doesn’t deliver just a few off numbers on a blood test. Energy crashes, foggy thinking, and stubborn weight come creeping back. Some patients chase their tails, switching dosages, never realizing morning routines need a tweak. One batch of labs might look fine, and then winter rolls in or someone starts a new round of supplements, and chaos returns. Nurses I’ve met in community clinics keep a laminated cheat sheet for patients so the message doesn’t get lost: “Don’t take anything but water with your thyroxine.”
Finding Good Solutions
Clear communication helps the most. A direct chat with a pharmacist can cut through confusion. Some people ask about a weekly pill box or reminders, but for thyroxine, daily focus wins out. Adjusting medication times—like flipping that calcium chew to an evening slot—can fix years of rollercoaster symptoms. Electronic health records with prompts add an extra layer of safety. In crowded clinics, a simple handout or text reminder reaches people who might not have time for a long conversation. With all the changes in medical guidelines, it’s easy to miss a small thing that makes a big difference. The key: regular follow-ups and an open line between patient, pharmacist, and doctor.
How long does it take for Thyroxine to start working?
Feeling Seen in Thyroid Troubles
People with hypothyroidism walk a tough road. The sluggish mornings, creeping weight gain, foggy thoughts, low mood—these symptoms don’t let anyone forget what’s missing. When a doctor hands over that prescription for thyroxine, hope rides alongside. But after starting those little white tablets, people naturally want to know: How long until things feel normal again?
Looking at the Science
Thyroxine isn’t a quick-fix drug. After taking a dose, it passes through the gut, travels in the blood, and eventually enters almost every cell. Each cell then uses it to run metabolism at a normal pace. The catch is, the thyroid hormones already in the body break down slowly. Some studies show it takes about a week for thyroxine blood levels to settle after starting treatment, but it may take up to six weeks to see a full response on blood tests and real-life symptoms. This timeline comes straight from major medical guidelines and endocrinologists who see hundreds of patients a year.
Why Changes Take Their Time
It’s tempting to think you’ll swallow a pill and feel different in days. The body rarely works like that. Fatigue often lingers, moods improve gradually, and skin can take months to get its normal glow back. This happens because tissues need time to catch up. Hair that started thinning last winter won’t thicken overnight. Plus, dosage adjustments aren’t rare. Doctors look at more than just the basic TSH blood test; they check free T4 and listen to symptoms. A safe approach means making slow changes and waiting at least a month before testing again.
Balancing Expectations and Monitoring
Patients deserve honest timelines. Some will notice more energy within two weeks. For others, the fog doesn’t lift for a month or even two. No single measure gives every answer. People who have lived with thyroid problems for years often need regular bloodwork, and their doctors may slightly change doses until the sweet spot arrives. That safe, slow process prevents heart problems and bone loss down the road. The American Thyroid Association stresses the importance of patience to avoid roller-coaster symptoms.
Supporting the Process
A pill solves the chemical problem, but it doesn’t fix everything. Exercise helps boost energy, even if it starts as a walk around the block. Iron and calcium can block thyroxine absorption, so waiting a few hours before eating those foods helps. Missing pills or taking the medicine at odd hours can cause symptoms to hang around. Clear communication with your provider provides the best shot at feeling well again.
Real-Life Stories Matter
Talking to others with thyroid disease helps. Support groups share stories and advice backed up by lived experience. Healthcare workers like pharmacists or endocrinologists see these struggles daily. They know it feels slow, but over time, most people do reclaim lost energy and focus. There’s comfort in knowing that, even though the journey isn’t speedy, science guides every step along the way.
| Names | |
| Preferred IUPAC name | (2S)-2-amino-3-[4-(4-hydroxy-3,5-diiodophenoxy)-3,5-diiodophenyl]propanoic acid |
| Other names |
L-thyroxine T4 Levothyroxine |
| Pronunciation | /θaɪˈrɒk.siːn/ |
| Preferred IUPAC name | 2-amino-3-[4-(4-hydroxy-3,5-diiodophenoxy)-3,5-diiodophenyl]propanoic acid |
| Other names |
L-thyroxine T4 Levothyroxine |
| Pronunciation | /θaɪˈrɒk.siːn/ |
| Identifiers | |
| CAS Number | 51-48-9 |
| Beilstein Reference | 421382 |
| ChEBI | CHEBI:30660 |
| ChEMBL | CHEMBL1132 |
| ChemSpider | 5461 |
| DrugBank | DB00451 |
| ECHA InfoCard | ECHA InfoCard 100.007.782 |
| EC Number | EC 228-287-7 |
| Gmelin Reference | 1631997 |
| KEGG | C01829 |
| MeSH | D013950 |
| PubChem CID | 5819 |
| RTECS number | YO8400000 |
| UNII | 8064XYD3TY |
| UN number | UN3249 |
| CAS Number | 51-48-9 |
| Beilstein Reference | 136815 |
| ChEBI | CHEBI:30660 |
| ChEMBL | CHEMBL1123 |
| ChemSpider | 5461 |
| DrugBank | DB00451 |
| ECHA InfoCard | 100.036.281 |
| EC Number | EC 1.14.99.3 |
| Gmelin Reference | 6131 |
| KEGG | C01829 |
| MeSH | D013930 |
| PubChem CID | 5819 |
| RTECS number | XO7975000 |
| UNII | N6HX2Q137E |
| UN number | UN3229 |
| CompTox Dashboard (EPA) | DTXSID2022853 |
| Properties | |
| Chemical formula | C15H11I4NO4 |
| Molar mass | 776.87 g/mol |
| Appearance | White, odorless, crystalline powder |
| Odor | No characteristic odor |
| Density | 1.3 g/cm³ |
| Solubility in water | Slightly soluble in water |
| log P | 4.3 |
| Vapor pressure | 0 mmHg (25°C) |
| Acidity (pKa) | 6.76 |
| Basicity (pKb) | 12.39 |
| Magnetic susceptibility (χ) | -32.6·10⁻⁶ cm³/mol |
| Dipole moment | 4.2928 D |
| Chemical formula | C15H11I4NO4 |
| Molar mass | 776.87 g/mol |
| Appearance | White, odorless, crystalline powder |
| Odor | Odorless |
| Density | 1.33 g/cm³ |
| Solubility in water | Slightly soluble in water |
| log P | 2.3 |
| Vapor pressure | Negligible |
| Acidity (pKa) | 6.79 |
| Basicity (pKb) | 5.85 |
| Magnetic susceptibility (χ) | -95.0·10⁻⁶ cm³/mol |
| Dipole moment | 3.5697 D |
| Thermochemistry | |
| Std molar entropy (S⦵298) | 564.5 J·mol⁻¹·K⁻¹ |
| Std enthalpy of formation (ΔfH⦵298) | -558.6 kJ·mol⁻¹ |
| Std enthalpy of combustion (ΔcH⦵298) | −8684 kJ/mol |
| Std enthalpy of formation (ΔfH⦵298) | -669.7 kJ·mol⁻¹ |
| Std enthalpy of combustion (ΔcH⦵298) | -7710 kJ mol-1 |
| Pharmacology | |
| ATC code | H03AA01 |
| ATC code | H03AA01 |
| Hazards | |
| Main hazards | May cause cancer; suspected of damaging fertility or the unborn child; harmful if swallowed; causes damage to organs through prolonged or repeated exposure |
| GHS labelling | GHS02, GHS07, GHS08 |
| Pictograms | GHS07, GHS08 |
| Signal word | Warning |
| Hazard statements | H373: May cause damage to organs through prolonged or repeated exposure. |
| Precautionary statements | Keep out of reach of children. Use only as directed by your physician. Do not use if allergic to levothyroxine sodium or any of the tablet's components. Store below 25°C, protect from light and moisture. |
| NFPA 704 (fire diamond) | 1-0-0 |
| Flash point | Flash point: 174.4°C |
| Autoignition temperature | 1160°C |
| Lethal dose or concentration | LD50 oral (rat) 100 mg/kg |
| LD50 (median dose) | LD50 (median dose): 100 mg/kg (oral, rat) |
| NIOSH | NO8245000 |
| PEL (Permissible) | 0.1 mg/m³ |
| REL (Recommended) | 50–200 micrograms per day |
| IDLH (Immediate danger) | Not established |
| Main hazards | May be fatal if swallowed, inhaled or absorbed through skin. |
| GHS labelling | GHS02, GHS07, GHS08 |
| Pictograms | GHS07 |
| Signal word | Warning |
| Hazard statements | H302: Harmful if swallowed. H373: May cause damage to organs through prolonged or repeated exposure. |
| Precautionary statements | Keep out of reach of children. Use only as directed by a physician. Store at controlled room temperature. Protect from light and moisture. Do not use if allergic to any ingredient. In case of overdose, seek medical attention immediately. |
| NFPA 704 (fire diamond) | 1-0-0-W |
| Flash point | Flash point: 113°C |
| Autoignition temperature | Unknown |
| Lethal dose or concentration | LDLo oral human 10 mg/kg |
| LD50 (median dose) | LD50 = 100 mg/kg (oral, rat) |
| NIOSH | WX1030000 |
| PEL (Permissible) | 0.1 mg/m³ |
| REL (Recommended) | Levothyroxine is the recommended preparation of thyroxine. |
| IDLH (Immediate danger) | Unknown |
| Related compounds | |
| Related compounds |
Triiodothyronine Diiodothyronine Reverse triiodothyronine Iodothyronine |
| Related compounds |
Triiodothyronine Reverse triiodothyronine Diiodothyronine |