Iodothyronine: A Down-to-Earth Look at an Endocrine Game-Changer
Historical Development
Digging into medicine's past, it’s clear that people recognized the power of iodine and thyroid extracts before scientists learned the details. Early healers treated swelling in the neck, or goiter, with burnt seaweed—a primitive but practical solution to iodine deficiency. Not until the late 19th century did researchers isolate thyroxine from animal glands, revealing the body’s dependence on specific iodine-containing molecules. The identification and synthesis of iodothyronines, including triiodothyronine (T3) and thyroxine (T4), carved a path for modern hormone therapies. These discoveries gave hope to those dealing with disorders like hypothyroidism. The journey from dried animal glands to pharmaceutical-grade tablets is lined with experiments, mistakes, and the stubborn determination of those chasing better health outcomes.
Product Overview
Iodothyronine stands as a cornerstone in the treatment of thyroid disorders. Unlike generic supplements, these synthetic hormones come with dosing precision and quality control. Pharmaceutical forms of T3 (liothyronine) and T4 (levothyroxine) support people dealing with hormone imbalances stemming from illness or thyroid removal. Authentic products display clear dosing charts, unique batch identifiers, and detailed safety information. These aren’t health fads—they form the backbone of essential therapies, giving users reliable symptom relief and a steady metabolic balance.
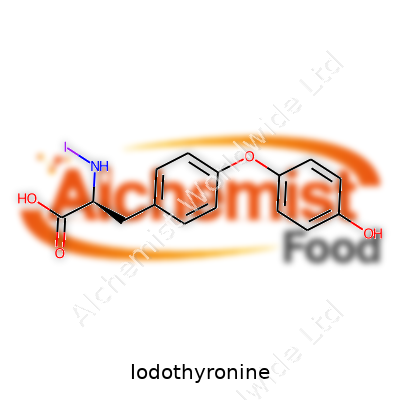
Physical & Chemical Properties
Iodothyronines show up as white to off-white crystalline powders that don’t blend into water but mix better with certain alcohols. With a melting point hovering around 232°C for T3, these compounds hold up well in tablet form, resisting easy degradation. Their chemical backbone features two rings—phenol and tyrosine—with iodine atoms securely attached. This setup grants selectivity, letting the body’s tissue-receptors “recognize” and respond to the hormone as if it were produced naturally. Stability matters, since light and moisture can degrade active compounds, so the pharmaceuticals industry invests in robust packaging.
Technical Specifications & Labeling
Pharmaceutical-grade iodothyronines alert users to potency, lot number, manufacturer, and expiration date. Labels draw attention to potential allergens and proper dosing instructions, so users and clinicians stay on track. Tablets or capsules ship in blister packs or bottles with tamper-evident seals and humidity absorbers. Every batch aligns with international pharmacopeia standards to ensure dose accuracy and uniformity across markets. This clarity doesn’t just satisfy regulations—it prevents life-altering dosing mistakes for people relying on thyroid replacement therapy.
Preparation Method
The bulk of pharmaceutical iodothyronine comes from well-controlled chemical synthesis rather than animal tissue. Manufacturers build the tyrosine backbone, add iodine atoms in measured steps, and purify the result with high-performance liquid chromatography. Rigorous solvent and impurity removal ensures a clean product. The end result must meet strict criteria before blending into tableted form with excipients that support shelf life. Scaling from laboratory technique to industrial production involves heavy oversight, regular equipment checks, and skilled technicians who know how to spot problems before anything reaches a pharmacy shelf.
Chemical Reactions & Modifications
Scientists can shift iodine atoms on the tyrosine scaffold, tweaking the biological activity and absorption rate. Removing iodine turns T4 into T3, which acts faster and leaves the body sooner. Chemical groups can be added to boost water solubility or slow absorption for special clinical uses. These modifications lend flexibility to hormone replacement regimens—important for people whose bodies handle hormones differently. Modern research investigates analogues that mimic natural hormones but dodge certain side-effects, aiming for more personalized endocrine care.
Synonyms & Product Names
In the pharmacy, iodothyronine might show up as liothyronine, levothyroxine, L-thyroxine, or simply T3 and T4. Big brands and generics share the market: Synthroid, Euthyrox, Cytomel are just a few. Researchers often use the chemical names, but patients see trade names depending on geography and distributor. Consistency in naming on packaging and prescriptions lowers chances of confusion—a key point when similar drugs differ in potency.
Safety & Operational Standards
Safety regulations around iodothyronine remain tough. Facilities must follow current Good Manufacturing Practice (cGMP). That means air filtration, worker training, regular audits, and full traceability from raw materials to finished product. Pharmacists and physicians read through clinical guidelines that outline safe starting doses, contraindications, warnings about drug-to-drug interactions, and side effect profiles. Regular blood tests check for over- or underdosing, because these hormones tightly control key body functions. Adverse event reporting systems catch issues in real-world use, prompting label updates and safer use practices.
Application Area
Doctors turn to iodothyronine to correct thyroid insufficiency, balance hormone levels after thyroid cancer surgery, or test for certain metabolic syndromes. In rare cases, it appears in clinical protocols for depression that's not responsive to standard therapies, though this use stays closely monitored. Endocrinologists count on it for fine-tuning metabolism in both children and adults. The role extends beyond humans—veterinarians use similar compounds to address thyroid issues in pets. My own encounter with these medicines came after a friend’s thyroidectomy; watching dose adjustments in real-time revealed just how critical these therapies are for normal energy, mood, and cognitive function.
Research & Development
Much of today’s research centers on better delivery methods and analogues that target specific tissues. Oral, transdermal, and even injectable options see investigation, with hopes for improved absorption and fewer side effects. Scientists dig into hormone transporters and cellular uptake, looking for ways to optimize dose and tailor therapy to individual patients. Genome research and “omics” data have started to shape thinking around who responds to which forms of hormone replacement. Health tech brings in digital tools for daily record keeping and faster dose cutbacks or increases, aiming for safer, patient-driven care management.
Toxicity Research
Clinical data demonstrates that toxicity from iodothyronine usually arises from dosing mistakes—over-replacement can induce rapid heart rate, nervousness, bone thinning, and in older adults, rhythm disturbances that risk cardiac events. Combating the risk means clear package coding and pharmacist counseling. Strict labeling and advised titration steps protect users. Since children handle thyroid hormones differently than adults, pediatric trials and decades-long monitoring have contributed to today’s safety standards. Temporary withdrawal or dose reduction often resolves minor toxicity, but severe cases demand ICU-level care. Toxicological studies continue to map the long-term outcomes from chronic high or low hormone states, informing future prescribing habits.
Future Prospects
New fronts open up as researchers look to integrate artificial intelligence and genetic insights into hormone replacement, building smarter dosing algorithms. Precision medicine may refocus therapy based not only on symptoms and labs, but also on genetic markers that predict how a person’s tissue will respond. Efforts to craft long-acting formulations, injectable microspheres, and targeted organ delivery draw big investment. Synthetic biology even points to potential for orally available, plant-derived hormone mimics. As more people live longer post-thyroidectomy and with metabolic disorders, the need for safer, more convenient hormone therapy keeps the field moving forward. Access and affordability will remain major hurdles, especially in low-resource settings where thyroid disease hits hard and steady medication supply can’t be taken for granted.
What is Iodothyronine used for?
Behind the Name: What is Iodothyronine?
Iodothyronines sound like something from a chemistry textbook, but they play a big part in energy and metabolism. These molecules, including two major forms—T3 and T4—come from the thyroid gland. I learned about these hormones when my cousin struggled with fatigue and weight changes, leading to a thyroid test that changed her life.
How Iodothyronine Affects Everyday Health
Iodothyronines act like the body’s regulators, influencing heart rate, temperature, mood, and even digestion. Thyroxine (T4) and triiodothyronine (T3) carry out jobs from cell repair to helping kids grow. A sluggish thyroid usually means not enough of these hormones. That comes with slow metabolism, brain fog, constipation, and sometimes hair loss. Too much, and people might deal with rapid heartbeat, anxiety, and sweating. My grandmother once called her overactive thyroid “living with a racing engine that won’t quit.”
Where Treatment Steps In
Doctors use iodothyronines mainly to treat underactive thyroid, or hypothyroidism. Levothyroxine, a synthetic version of T4, restores normal hormone levels. It helps millions get their energy and focus back. Endocrinologists have relied on this treatment for decades. A 2023 report from the American Thyroid Association pointed out that over 20 million Americans live with some form of thyroid disease, showing the need for effective thyroid hormone therapy.
Sometimes, T3 (liothyronine) joins the treatment plan for people who do not feel better with T4 alone. T3 works faster and has a stronger effect on the body, so it can lift stubborn symptoms in patients who stay tired or depressed even after regular levothyroxine doses.
The Big Picture: Why Everyone Should Care
Missing thyroid issues can cause big problems. Low levels in children stunt mental development, sometimes for life. Adults with untreated hypothyroidism live with fogginess and pain, then risk more serious heart problems down the line. I watched a neighbor’s health completely turn around after a simple thyroid supplement. She went from barely making it through the workday to hiking with her family on weekends. This isn’t rare—according to the National Institutes of Health, prompt thyroid hormone replacement helps people return to a regular, healthy life.
Challenges and Solutions in Thyroid Care
Not everyone finds relief right away. Sometimes, adjusting doses becomes a frustrating process. Blood tests measure thyroid hormones, but the most important sign for treatment remains how a person feels. Doctors keep watch for side effects, since too much T4 or T3 raises blood pressure and bone loss risk. Integrating routine thyroid checks into primary care visits helps catch problems before they become severe.
Many countries still struggle with iodine deficiency, cutting off the building blocks for these hormones. About a third of people worldwide do not get enough iodine, based on World Health Organization data. Adding iodized salt to diets wiped out most cases of deficiency in the US and Europe, proving that a small change can prevent big health issues.
Moving Forward with Smarter Choices
People often overlook thyroid health, chalking up tiredness or mood shifts to stress or age. Learning to ask for a thyroid test changed lives in my own family, and sharing these stories helps others do the same. Healthcare providers help most by listening—real stories matter more than textbook levels. Paying attention to symptoms plus routine testing offers the best shot at catching and treating problems early, leading to healthier, more active years for everyone.
How should I take Iodothyronine?
Sticking to Doctor’s Orders Matters
Nobody wakes up wanting a sluggish metabolism or shaky hands. Managing thyroid conditions calls for careful habits, especially with strong drugs like iodothyronine. I remember my uncle, always on his feet working construction, but suddenly he couldn’t get out of bed. Doctors found out his thyroid wasn’t keeping up. He got iodothyronine, but he learned the hard way you can’t play around with it—skipping pills, trying to double-up the next day, or mixing it with breakfast coffee didn’t do him any favors.
Timing Makes a Difference
Taking iodothyronine first thing in the morning with nothing else in your stomach opens the door for your body to soak it up. Swallowing it with water, not milk or juice, follows the advice of serious endocrinologists. Even calcium pills or iron supplements can block some of the medicine before your bloodstream gets a chance. Some people figure once a day means whenever they remember, but that back-and-forth turns the body’s hormone levels upside down. It helps to pick a time—like soon as you wake up—and stick with it. The body likes routines, and so do the lab numbers.
Why Skipping Doses Isn’t Harmless
Forgetting a dose might not seem urgent, but the thyroid runs like a factory line. The pituitary gland pays attention and reacts if the supply drops. Some folks might feel tired, others notice their heart speeding up. There’s real science behind this: thyroid hormone keeps your energy, brain, and heart moving at the right pace. Big swings in hormone levels can shake everything loose—your mood, sleep, blood pressure. That’s not a risk worth taking.
Side Effects—Not Just in Textbooks
Real people get nervous hands, sweating, or headaches if the dose climbs too high. Others say their heart skips or sprints. These reactions put a strain on older adults or anyone with a weak heart. It’s not fearmongering, just personal experience and a dose of respect for a strong drug. I watched my neighbor, thinking she could “speed up” weight loss by taking extra pills. It landed her in the ER—lesson learned: more is not better with thyroid medicine.
Fine-Tuning Takes Teamwork
Good doctors watch blood work closely and adjust doses. No two people run the same, so copying someone else’s schedule makes little sense. Keeping regular appointments and talking about every symptom—good or bad—helps the doctor make smarter choices. Internet advice or family rumors rarely match the care a provider delivers. Bringing a list of other prescriptions or natural supplements helps, too. Drug interactions sneak up quickly, especially with heart pills or diabetes treatments.
Solutions Backed by Experience
Good habits start with setting reminders—an alarm, sticky notes, or a pillbox on the nightstand. Asking questions isn’t a sign of weakness; it clears up dangerous mistakes. Keeping food, vitamins, and other pills apart from iodothyronine, unless a healthcare provider says otherwise, helps your body get the full benefit. There’s comfort in routine and trust in real-life guidance.
What are the possible side effects of Iodothyronine?
What Happens After Taking Iodothyronine?
Doctors prescribe iodothyronine, also known as liothyronine, mostly for people struggling with low thyroid function. This medication can turn things around, often delivering energy back to folks used to feeling tired all day. As with any medication, taking it opens the door to possible side effects. Some show up early, others take time to reveal themselves. Knowing what to look for can keep surprises at bay and help prevent bigger problems down the road.
The Common Physical Symptoms
Most people start with the basics. After starting iodothyronine, somebody might notice a racing heart or an uneasy chest. Sweating without much activity, feeling warm even in winter, shaky hands, or anxiety creep up suddenly. Sleep can turn into a hassle: tossing, turning, mind racing at 2 a.m. Instead of sluggishness, people sometimes feel wired—too much of a good thing. For folks dealing with heart trouble, palpitations become risky. A rapid pulse isn’t just uncomfortable; it can spell danger.
Mood and Mental Health Shifts
An overlooked piece of the puzzle sits with mood swings. Lifting brain fog feels like a blessing, but swinging into irritability or hyperactivity raises new problems. Real stories echo across clinics: bursts of frustration, restlessness, or panic attacks out of nowhere. Over time, these can strain relationships and work life, especially if no one suspects the thyroid pill as the trigger.
Digestive System Tells Its Own Story
People sometimes ignore their gut, chalking up issues to bad food or stress. With iodothyronine, the metabolism picks up speed. Food moves faster. Diarrhea or more frequent trips to the bathroom follow. Some start losing weight without trying—sounds nice at first but turns concerning if muscle disappears and energy tanks. Even the appetite jumps around: some days everything tastes amazing, other times food loses its appeal.
Long-Term Concerns and Special Cases
Pushing the thyroid too hard carries risks. Over months or years, bones give up their strength when metabolism never gets a break. Fractures start showing up in people far from old age. Calcium starts leaking out of bones, thinning them out quietly. For older adults or anyone who already faces bone loss, this matters a lot. A few end up with irregular heartbeats that stick around, sometimes leading to hospital visits.
Who Faces the Biggest Risks?
Some groups find themselves in tighter spots. People with a history of heart disease walk a thin line—too much thyroid hormone, and complications sprout. Age plays a part; older bodies recover slower, and side effects pack a bigger punch. Pregnant folks need careful monitoring, since the right level helps both parent and baby, but the wrong dose can cause trouble for the unborn child.
Practical Steps for Safety
Open conversation with a healthcare provider keeps risks in check. Blood tests track progress: TSH and T3 levels, heart rhythm, bone strength. Reporting symptoms—no matter how small—can prompt tweaks that keep benefits without as many side effects. Some patients keep a diary to spot changes early. Sticking with regular check-ins helps spot big problems before they grow. Taking the lowest dose that works remains the safest bet, and skipping the temptation to self-adjust means fewer surprises.
Smart Choices Make a Difference
Medication like iodothyronine changes lives for many. Respecting the flip side—these side effects—gives people and their doctors better tools to balance energy, mood, and long-term health. Honest attention to symptoms, steady monitoring, and trusting a well-informed medical team lay out the clearest path for those who need thyroid help.
Can Iodothyronine interact with other medications?
Looking Beyond Labels
Picking up a bottle of iodothyronine from the pharmacy, you might not think much about what happens after you swallow a dose. Most of us just want to manage our thyroid symptoms and get on with our lives. Still, combining iodothyronine with other regular prescriptions changes that whole picture.
Mixing Medications Means More Than Guesswork
Talking about interactions might sound dry, but it matters—especially to people juggling pills every morning. I learned about these risks firsthand. My dad, after years on thyroid therapy, landed in the ER with heart palpitations. No one warned him that a new antidepressant could crank up his thyroid hormone activity. Only after testing did his doctor connect the dots.
It's easy to overlook small pills, but iodothyronine does not work alone. It runs your body’s energy machine, governing metabolism, heartbeat, and even your mood. Throw another medication into the mix, and things can get unpredictable.
Not Just a Pharmacy Problem
Doctors are the first line of defense but don’t always see the full picture. Many folks see multiple specialists who prescribe pills without always checking current medications. Research backs this up: according to an article in the Journal of Clinical Endocrinology & Metabolism, about one in five people on thyroid medications gets affected by another drug's interference.
Take blood thinners like warfarin. Iodothyronine speeds up their breakdown, leading to lower blood levels and increased stroke risk. On the other side, cholesterol drugs such as cholestyramine latch onto iodothyronine in your gut, keeping it out of your bloodstream. Even over-the-counter antacids mess with absorption. It’s no wonder people might feel dizzy, tired, or jittery without knowing why.
Why It Matters for Everyday Life
Driving to work, taking care of family, and planning for a regular day relies on a body that isn’t throwing off warning signals. Uncontrolled thyroid levels can raise the risk of arrhythmias, bone loss, and even cognitive changes. For seniors, that means falling or confusion; for younger people, that adds unnecessary fog to already busy days.
Mixing up the order you take pills, skipping breakfast, or even changing brands might throw off balance. Making matters stickier, supplements like iron and calcium have a reputation for blocking iodothyronine absorption, sneaking in side effects, and leaving patients and doctors scratching their heads.
A Few Smarter Habits
Staying safe doesn’t require a medical degree. Most important advice many pharmacists give—bring your full medication list every check-up. Don’t guess or rely on memory. Use one pharmacy for all refills to catch possible clashes. Ask direct questions: “Will any of my medications interfere with this prescription?” Jot down each doctor’s name and connect everyone involved with your care.
Food can also trip you up. Caffeine, grapefruit juice, and certain high-fiber choices can all shift hormone levels. Scheduling your iodothyronine dose with water, at the same time each day, keeps things steady.
Partnering With Your Health Team
Living well on thyroid therapy calls for partnership. Keeping a written log, updating it after every new prescription, and sharing concerns—even those that seem minor—builds a better safety net. Beyond that, reading reliable sources like the Mayo Clinic or Endocrine Society provides up-to-date answers. Few things beat the peace of mind that comes with double-checking before trouble starts.
Is Iodothyronine safe during pregnancy or breastfeeding?
Understanding Iodothyronine and Its Role
Iodothyronine covers hormones like T3 and T4, which drive much of the human body's metabolism. These hormones support brain growth, regulate energy, and play a role in keeping the body’s systems running smoothly. In pregnancy and breastfeeding, a woman’s thyroid carries extra weight: the right balance of these hormones supports a baby’s brain, heart, and skeletal growth.
Risks of Taking Extra Iodothyronine
Doctors tend to prescribe iodothyronine, including liothyronine (T3) or levothyroxine (T4), for people with an underactive thyroid gland. Pregnancy itself puts a greater demand on thyroid hormones. Thyroid dysfunction poses real threats: too little causes miscarriage risk, premature birth, and problems in a child’s intelligence and motor skills; too much pushes up blood pressure, triggers heart strain, and risks abnormal birth weights or preterm labor.
Supplementing with iodothyronine ought to only happen under a doctor’s watch. Over-supplementation may tip the scales towards hyperthyroidism. Babies of mothers with excess thyroid hormone can develop irritability, fail to gain weight normally, even have abnormal skull closure or birth defects. Health authorities such as the U.S. Food and Drug Administration and European guidelines both caution about taking thyroid hormones without strict medical guidance during pregnancy and breastfeeding.
Facts From Research and Real-World Medical Practice
Doctors rely mostly on levothyroxine, the synthetic form of T4, for pregnant patients who need thyroid hormone support. T3 (liothyronine) does not cross the placenta efficiently. The fetus receives most of its early thyroid hormone in the form of T4, which it later converts to T3. Extra T3, especially without medical need, brings more harm than help. That’s why independent use, go-it-alone supplements, or alternative blends from overseas suppliers almost always carry unnecessary risks.
Research in the journal Clinical Endocrinology finds that women who controlled their hypothyroidism with levothyroxine had the best odds for healthy outcomes, but overdose and fluctuations create real problems. If a woman has known thyroid disease, doctors track TSH and free T4 every 4 to 6 weeks. This routine monitoring lets them fine-tune the dose for both mom and baby’s safety.
What About Breastfeeding?
Breastfeeding moms still need enough thyroid hormone, for themselves and for milk production. The American Thyroid Association says that standard doses of levothyroxine remain safe in breastfeeding. Milk can carry tiny traces of T4, but not at levels that threaten a baby. High doses or unregulated use could pass on too much, though, which could unsettle an infant’s own delicate system.
Navigating Uncertainty: Practical Steps
If thyroid testing shows something’s off during prenatal visits, communicate and push for a clear treatment plan. Don’t tinker with herbal remedies or online supplements marketed as “thyroid boosters.” Pregnancy and new motherhood both make the body’s demands go up, but more isn’t always better when it comes to hormones. The right balance takes working with trustworthy care teams, leaning on labs and well-established drug safety data.
Thyroid conditions in pregnancy and breastfeeding can feel overwhelming. Solid facts show that managed hormone replacement, at the lowest dose needed, brings the best results. Medication only belongs in the picture because a qualified healthcare provider says so. That’s the path science, patient stories, and decades of clinical results keep backing up.
| Names | |
| Preferred IUPAC name | 3-iodo-4-(4-hydroxy-3-iodophenoxy)phenol |
| Other names |
Diiodothyronine Triiodothyronine Tetraiodothyronine Thyronine derivatives |
| Pronunciation | /ˌaɪ.oʊ.doʊˈθaɪ.rəˌniːn/ |
| Preferred IUPAC name | 3-iodo-1,3-dihydro-1-[(4-hydroxyphenyl)methyl]-4H-imidazol-4-one |
| Other names |
Iodothyronines Thyronines |
| Pronunciation | /ˌaɪ.ə.dəʊ.θaɪˈroʊ.nin/ |
| Identifiers | |
| CAS Number | 6893-02-3 |
| Beilstein Reference | 3766054 |
| ChEBI | CHEBI:25037 |
| ChEMBL | CHEMBL1548 |
| ChemSpider | 11036 |
| DrugBank | DB00279 |
| ECHA InfoCard | 03c0b8d9-6e5b-4a7b-a0bb-fb2e88572c09 |
| EC Number | 3.1.1.54 |
| Gmelin Reference | 93898 |
| KEGG | C08360 |
| MeSH | D007478 |
| PubChem CID | 9562 |
| RTECS number | NL1672000 |
| UNII | 21X6J9B0ZE |
| UN number | UN3270 |
| CAS Number | 6893-02-3 |
| Beilstein Reference | 3567556 |
| ChEBI | CHEBI:25005 |
| ChEMBL | CHEMBL1640 |
| ChemSpider | 5577 |
| DrugBank | DB00279 |
| ECHA InfoCard | 14b5df68-d8d9-47ef-9bfc-9427c9056d44 |
| EC Number | 3.8.1.4 |
| Gmelin Reference | 96378 |
| KEGG | C02463 |
| MeSH | D007468 |
| PubChem CID | 9555 |
| RTECS number | NL2275000 |
| UNII | VM6OU04Z3Z |
| UN number | UN3271 |
| CompTox Dashboard (EPA) | DTXSID0024743 |
| Properties | |
| Chemical formula | C15H11I3NO4 |
| Molar mass | 777.96 g/mol |
| Appearance | white to off-white crystalline powder |
| Odor | Odorless |
| Density | 1.55 g/cm³ |
| Solubility in water | Insoluble in water |
| log P | 4.97 |
| Vapor pressure | 4.5E-10 mmHg |
| Acidity (pKa) | 8.53 |
| Basicity (pKb) | 4.19 |
| Refractive index (nD) | 1.786 |
| Dipole moment | 4.44 D |
| Chemical formula | C15H11I3NO4 |
| Molar mass | 650.97 g/mol |
| Appearance | White to off-white crystalline powder |
| Odor | Odorless |
| Density | 1.55 g/cm³ |
| Solubility in water | Very slightly soluble in water |
| log P | 2.5 |
| Vapor pressure | 6.59E-13 mm Hg |
| Acidity (pKa) | 8.5 |
| Basicity (pKb) | 6.76 |
| Magnetic susceptibility (χ) | -94.0e-6 cm³/mol |
| Refractive index (nD) | 1.672 |
| Dipole moment | 3.1745 D |
| Thermochemistry | |
| Std molar entropy (S⦵298) | Std molar entropy (S⦵298) of Iodothyronine: 519 J·mol⁻¹·K⁻¹ |
| Std molar entropy (S⦵298) | Std molar entropy (S⦵298) of Iodothyronine is 610 J·mol⁻¹·K⁻¹ |
| Pharmacology | |
| ATC code | H03AA02 |
| ATC code | H03AA02 |
| Hazards | |
| Main hazards | May cause irritation to skin, eyes, and respiratory tract. Harmful if swallowed or inhaled. |
| GHS labelling | GHS07, GHS08 |
| Pictograms | GHS07 |
| Signal word | Warning |
| Hazard statements | H302: Harmful if swallowed. H373: May cause damage to organs through prolonged or repeated exposure. |
| Precautionary statements | P264, P270, P273, P280, P301+P312, P305+P351+P338, P330, P501 |
| NFPA 704 (fire diamond) | 1-1-0 |
| Flash point | Flash point: 113.5°C |
| Autoignition temperature | Autoignition temperature: 500°C |
| Lethal dose or concentration | Iodothyronine: LD50 (rat, oral) > 2000 mg/kg |
| LD50 (median dose) | LD50=852mg/kg (oral, rat) |
| NIOSH | WZ2625000 |
| PEL (Permissible) | Not established |
| REL (Recommended) | 65–130 micrograms daily |
| IDLH (Immediate danger) | No IDLH established. |
| Main hazards | May cause irritation to eyes, respiratory system and skin. |
| GHS labelling | GHS07, GHS08 |
| Pictograms | GHS07 |
| Signal word | Warning |
| Hazard statements | H302: Harmful if swallowed. H373: May cause damage to organs through prolonged or repeated exposure. |
| Precautionary statements | Wash thoroughly after handling. Do not eat, drink or smoke when using this product. IF SWALLOWED: Immediately call a POISON CENTER/doctor. Rinse mouth. Dispose of contents/container in accordance with local/regional/national/international regulations. |
| Flash point | 80°C |
| Lethal dose or concentration | LD50 intravenous (rat) 61 mg/kg |
| LD50 (median dose) | LD50: 820 mg/kg (oral, rat) |
| NIOSH | PY9945 |
| PEL (Permissible) | 0.1 mg/m3 |
| REL (Recommended) | 50–100 mcg daily |
| IDLH (Immediate danger) | Not established |
| Related compounds | |
| Related compounds |
Iodothyroacetate Thyroid hormone Iodotyrosine |
| Related compounds |
Thyroxine Triiodothyronine Reverse triiodothyronine |