Ferrous Fumarate: A Closer Look at an Iron Supplement Mainstay
Historical Development
Discovery and commercial use of ferrous fumarate trace back to a time when doctors sought more tolerable iron sources for treating anemia. Traditional iron salts, like ferrous sulfate, caused gastrointestinal distress for many patients. Researchers began to explore alternatives that would offer higher bioavailability alongside better patient comfort. Fumaric acid, isolated from lichens and later synthesized from maleic acid, entered pharmacological conversation during the 20th century. Chemists soon reacted it with iron(II) salts, resulting in ferrous fumarate. By the late 1960s and early 1970s, over-the-counter iron supplements adopted this compound. Its rise was driven by ease of manufacture, affordability, and an improved experience for patients, which encouraged widespread medical use.
Product Overview
Pharmacies and supplement shelves today tend to include products packed with ferrous fumarate, defined as Iron(II) salt of fumaric acid. Manufactured either as tablets, capsules, or sometimes powder for suspension, manufacturers focus on precise elemental iron content, which sits just above thirty percent by weight. The supplement provides a means to restore iron stores in people facing iron deficiency anemia, especially prevalent among pregnant women, young children, and individuals with chronic blood loss. Beyond prescription or over-the-counter sales, food fortification programs in public health settings rely on it, especially in flour, cereals, and nutrition bars.
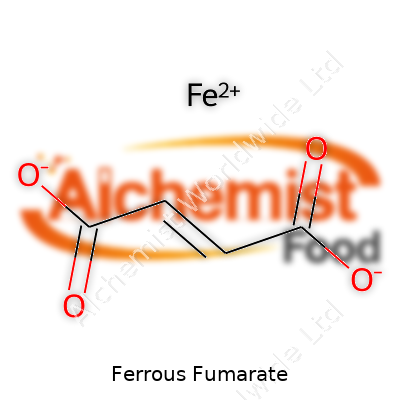
Physical & Chemical Properties
Ferrous fumarate appears as a reddish-orange powder, barely soluble in water, but stable in dry air. Moisture, on the other hand, slowly oxidizes the ferrous ion to ferric iron, altering both effectiveness and shelf life. It carries a molecular formula of C4H2FeO4 and a molar mass near 169.9 g/mol. Unlike ferrous sulfate, the taste tends to be less metallic, and gastric irritation seems reduced according to user feedback and clinical reports. A key property involves its slow oxidation, which benefits shelf stability and reduces risk of taste changes in fortified foods.
Technical Specifications & Labeling
Manufacturers usually standardize elemental iron content with rigorous batch testing, aiming for declared iron levels that match the product’s claims. Pharmacopoeias in regions like Europe, the US, and Asia all specify accepted methods for purity testing, residue on ignition, loss on drying, and absence of common contaminants such as lead, mercury, and arsenic. Labels need to show the exact content of elemental iron, clearly distinguish ferrous fumarate from other forms of iron, and carry warnings about overdose and potential poisoning risks—especially relevant in environments with children at home. Traceability, manufacturing lot number, expiry dates, and storage guidance count as non-negotiable requirements, building trust with both clinicians and consumers.
Preparation Method
Industrially, producers react highly pure fumaric acid with iron(II) ions, usually sourced from ferrous sulfate or ferrous acetate. The process often gets carried out in aqueous media at controlled temperature and pH, ensuring consistent precipitation of the metal-organic salt. After mixing, the product gets filtered, washed multiple times to strip away excess reactants and soluble impurities, and then dried thoroughly under vacuum or in low-humidity rooms. Manufacturers sometimes micronize the powder to improve blending in tablet or capsule formulations. This manufacturing method supports large-scale, cost-effective production with minimal environmental discharge.
Chemical Reactions & Modifications
Ferrous fumarate’s main reactivity in a pharmaceutical sense involves mild acid dissociation, which releases iron ions in the stomach’s acidic environment. Stomach acid breaks ferrous fumarate down into its components, freeing Fe2+ for absorption. Chemists do sometimes use coating strategies, encapsulating the compound, to control release or shield the iron from unwanted oxidation before ingestion. When exposed to air and moisture, the iron(II) part begins converting into less soluble and less absorbable iron(III), a factor that sets boundaries for storage, packaging, and shelf life. Producers work to manage this with desiccants and opaque containers, aiming to slow down degradation.
Synonyms & Product Names
Ferrous fumarate carries several alternative names, such as iron(II) fumarate, fumaric acid iron(II) salt, and in some texts, simply "fumarate iron." Major global brands include Ferro-Sequels, Ferretts, and various generics available in dozens of countries. In non-pharmaceutical contexts, it sometimes surfaces simply as "fumarate, iron." For those hoping to identify the compound in international trade, the CAS number 141-01-5 becomes a useful reference, often signaling compliance across different regulatory borders.
Safety & Operational Standards
Strict standards guide the production and handling of ferrous fumarate. Workers handle bulk synthesis within controlled-air plants, wearing protective gear against iron dust exposure. Occupational Safety and Health Administration (OSHA) guidelines mark iron compounds as hazardous, so ventilation systems, dust collection, and routine air monitoring become standard. Fire isn’t a huge concern, but operators avoid high humidity and direct sunlight to prevent premature oxidation. Companies must record batch samples for years, and adhere to regular third-party audits, guaranteeing a safe supply chain. Consumer safety hinges on clear overdose warnings and poison control advice printed on every label.
Application Area
Ferrous fumarate’s job as a supplement goes beyond treating anemia in clinics. Public health programs looking to tackle nutritional iron deficiency often use this compound in fortified foods and even ready-to-use therapeutic foods for malnourished children. Doctors tend to pick it for patients with chronic kidney disease because it fits well in most clinical protocols and is less likely to upset digestive systems. Nutraceutical firms add it to multivitamins and prenatal formulations. In the food industry, some bakers rely on it to enrich bread, biscuits, and breakfast cereals, capitalizing on its color stability and low impact on flavor. Animal feed manufacturers occasionally employ it to boost livestock health, especially in regions wrestling with soil iron deficiency.
Research & Development
University labs and pharma companies continue to probe ferrous fumarate’s pharmacokinetics and bioavailability. Work goes into novel tablet coatings, which might protect iron from GI tract oxidation or prevent interaction with calcium-rich foods. Some teams experiment with probiotic-iron hybrid supplements, hoping to maximize uptake while side-stepping the common digestive woes. Studies in fortification science examine synergistic blends—adding vitamin C or certain amino acids to formulations, aiming for a better uptake in the small intestine. Research into microencapsulation technology promises to solve taste, stability, and compatibility problems for food-grade applications.
Toxicity Research
No element brings benefit without risk, and iron certainly fits that rule. Accidental overdose of supplements—particularly in young children—presents as a leading cause of fatal poisoning in some regions. Early signs range from nausea and abdominal pain to liver failure and metabolic acidosis. Because of these dangers, toxicologists examine not just acute but also chronic low-level exposure, checking for oxidative stress, organ damage, and interactions with other medications. Long-term animal studies help regulators set clear upper limits for safe intake. Surveillance of poison control data prompts tweaks to packaging and labeling, especially those child-resistant bottle caps and warning icons which have now become a global standard in the industry.
Future Prospects
The search for safe, sustainable, and effective iron supplementation keeps driving fresh innovation. Modern life, with its shifting dietary patterns and continued public health challenges, keeps demand for improved supplements alive. Technology may unlock new delivery systems—perhaps slow-release forms suited to those with sensitive digestion, or smarter blends pairing iron with absorption boosters tailored for vegetarian diets. Fortification science stands ready to move beyond cereal grains, finding new vectors for reaching at-risk populations, from plant-based beverages to clinical nutrition formulas. Ultimately, the world’s iron needs point toward a future where every child and adult, regardless of circumstance, can access reliable, safe sources—ferrous fumarate will likely remain in that toolbox for years yet.
What is Ferrous Fumarate used for?
Understanding Ferrous Fumarate
Ferrous fumarate gives people a reliable way to boost iron intake, especially during times in life when bodies ask for more than usual. This supplement has earned its spot in medicine cabinets and clinic drawers because iron deficiency can drain energy and lead to problems with growth, learning, and basic daily functions. In my own experience working with patients in both rural and urban clinics, I've seen how iron supplements turn around lives that anemia has complicated.
Iron keeps blood healthy. Without enough, red blood cells struggle to carry oxygen. The body starts sending distress signals: tiredness, trouble focusing, shortness of breath, and in severe cases, odd cravings for things like ice or clay—symptoms doctors see too often, especially in teenagers, pregnant people, and busy adults who skip meals. Ferrous fumarate delivers iron in a form that the body handles better than some other supplements.
Why Some Groups Depend on This Supplement
Pregnancy changes iron needs rapidly. Blood volume rises and the body builds a support system for a growing child. Women who carry twins or multiples end up needing even more. If these needs go unmet, risks grow—not just for tiredness or paleness, but for early delivery or low birthweight. Doctors almost always recommend an iron supplement, and ferrous fumarate stays near the top of the list because it balances strong absorption with a side effect profile patients manage.
Children, especially picky eaters or kids from families struggling to put enough food on the table, can fall behind in their growth or struggle with attention in school because they're running low on iron. I’ve worked in food banks and noticed many nutrition programs include iron-fortified foods or drops with ferrous fumarate to help bridge this gap. Sometimes families don’t catch iron deficiency until a teacher or coach mentions lagging performance or unusual fatigue.
Some adults—vegetarians, people who donate blood often, or those with digestive issues—also benefit from an added iron source. The supplement isn’t a cure-all, but it gives many people a practical way to cover a basic nutritional need. Every year, thousands of people find out their exhaustion isn’t just stress, but a simple lack of iron, solved with a daily dose.
The Hidden Risks and How to Handle Them
Ferrous fumarate can cause trouble if used carelessly. Taking too much iron can upset the stomach or lead to constipation. Some people give up after a few days because they think the discomfort outweighs the benefits. I’ve heard patients say the medicine ‘didn’t agree with them,’ which usually means nobody told them mixing the tablet with food or switching to a lower dose could make things easier. Open conversations about these issues keep people from abandoning treatment too soon.
For families with small children, safe storage matters. Kids who eat iron tablets by accident can end up in the emergency room—unintentional poisoning with iron stands as a real, serious risk. Simple steps, like using bottles with child-resistant caps and keeping medicine out of sight, save lives.
Building Better Awareness
Most people don’t know which foods bring in the most iron, or that coffee, tea, and certain antacids block absorption. Health professionals, schools, and community groups can step in to close these knowledge gaps. Better awareness turns a simple supplement like ferrous fumarate into a powerful tool for health, not just another pill to collect dust on a shelf.
Doctors have to tailor dosing, check interactions, and review lab results to make sure people use ferrous fumarate safely and get the intended benefit. As more research comes out and public health programs reach those at higher risk, this humble supplement proves its value every day in practices big and small.
How should I take Ferrous Fumarate?
What Ferrous Fumarate Does for You
Most people don’t realize how low iron sneaks up on you. Feeling tired, catching your breath too fast on the stairs, dull skin, or even headaches can be part of it. A doctor might check your blood and say you need more iron. Ferrous fumarate brings your levels back up. This medicine feeds your body what it’s missing, usually after blood loss, heavy periods, or stubbornly low iron from food.
Getting the Most From Your Tablet
Doctors recommend ferrous fumarate because it’s reliable. But your body absorbs iron weirdly. It grabs more on an empty stomach, but not everyone handles that well. If taking it before food feels rough, eat a small snack—not dairy, no coffee, no tea. Calcium, black tea, coffee, and antacids block iron. Orange juice gives iron a hand. It’s Vitamin C, pure and simple. I learned that squeezing a clementine over breakfast goes a long way for my energy, and it makes the routine less of a chore.
Gulp your pill down with water. Big multivitamins or other meds compete for attention, so keep iron apart from those by two hours. Sometimes, doctors suggest one pill a day, sometimes twice: follow their plan, not your friend’s. Too much iron never does your gut any favors.
What to Expect and How to Handle Side Effects
Iron, especially the ferrous kind, can be tough on the stomach. Some folks get constipation, odd stomach aches, or even feel queasy. If you do, don’t just quit it. Up your water, bring in more fiber, and walk around more. Over time, most stomach problems melt away. And don’t be alarmed: your stool might turn dark. Nothing dangerous, just a sign the iron’s working.
Missing a dose happens, but don’t double up the next time. Just keep going as usual. It’s no reason to get anxious. Your doctor tracks your progress with blood tests, so keep appointments and share anything unusual. Some people need long-term iron, others only a short boost. Good communication with your provider matters.
Why Proper Iron Use Matters
Iron deficiency runs deeper than tiredness. Pregnant women and young children need enough iron for brain growth and keeping infections away. In my own family, we’ve seen how kids perk up after a few weeks of the right supplement. But too much iron builds up, hurting the liver and heart. So, avoid random iron pills from the corner store if your doctor hasn’t called for it.
Around the world, iron deficiency causes more than half of all anemia cases, especially where food choices are limited. It drags down school results, work life, pregnancy outcomes, and leads to preventable deaths. Recognizing symptoms early, choosing the right treatment, and using plain old food tips alongside medicine builds a stronger, healthier person. Simple routines make all the difference.
Simple Steps for Better Results
Iron pills won’t fix everything overnight, but steady use brings energy back. Pair your supplements with fruit or veggies rich in Vitamin C. Avoid rivals like tea, coffee, and high-calcium foods around pill time. Track your side effects and talk openly with your healthcare team. Iron’s not just a number in your labs—it's key to everything you do. Tackle low iron head-on. Good advice, smart habits, and a little patience will pay you back in days you feel brighter and ready for anything.
What are the possible side effects of Ferrous Fumarate?
Iron Pills Don’t Always Go Down Easy
Taking ferrous fumarate brings plenty of people relief from the low energy and foggy brain that come with iron deficiency. Pop the pill, expect more pep—then your stomach jumps in with a different plan. Cramps, queasiness, and trips to the restroom can take center stage. Constipation pops up often, even for folks who usually have clockwork digestion. Sometimes, that constipation swings in the opposite direction and diarrhea shows up. It’s frustrating sitting through both sides, trying to figure out which end will give in first.
More Than a Bit of Discomfort
My experience with iron supplements started a few winters ago. My body ached, my mind dragged, and the doctor’s fix was iron. A week in, I felt like my stomach was throwing a tantrum every time I swallowed that rusty-tasting pill. Nausea rolled in most mornings. My appetite vanished almost as quickly as my patience. Strange as it sounds, that infamous black stool really surprised me at first—but it pops up often with iron pills, including ferrous fumarate.
Plenty of friends and patients have told me about the same rollercoaster. One had stomach pain so fierce, she almost stopped taking the pills even though her bloodwork screamed for them. Others dealt with a permanent taste of metal in their mouths. Rarely, someone breaks out in hives or has trouble breathing. Allergic reactions are less common, but they mean a trip to urgent care. Some folks describe feeling weak or dizzy, which is odd when you consider they started the supplement to beat fatigue. It’s hard to trust iron to do its thing when the side effects knock the wind out of you.
Why Do the Side Effects Hit Hard?
Ferrous fumarate sits right up there with other iron supplements in terms of causing digestive drama. Iron irritates the stomach lining. Our guts can only absorb so much. What you don’t absorb, you excrete—and that leftover iron churns up the intestines. Research shows about one in five people who take iron pills complain about stomach upset or bowel problems. The World Health Organization says that a small percentage will drop the supplement completely because the symptoms mess with their day so badly.
Blood in the stool or sharp, unrelenting cramps signal that you need to call a doctor. Low iron is a problem, but gut bleeding is a bigger one. Anyone with a history of stomach ulcers should talk with their provider from the start.
Tweaking How You Take It
Small changes can make things smoother. Split up the daily dose. Take it with food, even though that takes the edge off absorption. Vitamin C can help your body snag more of the iron, so orange juice makes a better companion than coffee. Doctors sometimes suggest a lower dose or a slow-release tablet for people who really struggle. If constipation runs wild, fiber and extra fluids do a world of good. A gentle stool softener works for some.
People shouldn’t play guessing games with supplements. Open talk with a healthcare provider does more than just troubleshoot annoying symptoms. It catches big problems early and shapes a safer plan—one that lifts energy without turning your stomach into an enemy.
Looking at research, iron deficiency is no small problem—almost a third of the world faces it at some point. Ferrous fumarate makes a difference, as long as you’re ready for a few bumps along the way and talk honestly about what your body’s telling you.
Can I take Ferrous Fumarate during pregnancy or breastfeeding?
Nourishing Two Lives with Iron
Pregnancy flips your diet and supplement routine upside down. For many, doctors prescribe ferrous fumarate—a simple iron supplement. Anyone who’s felt that wave of tiredness during pregnancy probably knows a thing or two about iron deficiency anemia. I remember dragging myself to the fridge one morning, lightheaded and foggy. Blood tests confirmed my iron was running low, and my midwife scribbled “ferrous fumarate” on a slip. The stuff matters, especially since a pregnant body uses a lot more iron. Growing a baby isn’t a small job, and iron helps carry oxygen in your blood. It’s not just for the baby—your own body relies on it to push through those long months.
Why Extra Iron Sometimes Makes Sense
Doctors don’t dish out iron pills for fun. Almost half of pregnant women around the world end up dealing with low iron, according to the WHO. Iron-deficiency anemia raises the risk of early labor, low birth weight, and slower brain development in newborns. Despite every best intention, it gets tough to eat enough spinach or red meat every day to keep up, especially if morning sickness or food aversions hit. That’s where supplements like ferrous fumarate step in. Decades of research show that when bloodwork confirms deficiency, these pills do the job—usually without fuss if you take them with food to dodge stomach problems.
Understanding Risks and Managing Side Effects
Most iron supplements list nausea or constipation as side effects. Ferrous fumarate isn’t magical—it’s the same. I’ve had friends who couldn’t handle it without a snack, or who needed to switch brands. Nobody needs to suffer through gassy afternoons or stubborn bowels. Drinking lots of water or adding fiber can ease the ride. While we can trust ferrous fumarate's safety, don’t pop extra pills for the sake of it. Too much iron causes its own set of problems. Follow the dose on your prescription or advice from your healthcare provider.
What About Breastfeeding?
After birth, iron stores take a hit—thanks to blood loss and handing all those nutrients over to the new baby. Breastfeeding moms still need plenty of iron, especially right after delivery. Studies confirm that using ferrous fumarate after birth fills up iron reserves safely. The body uses what it needs; there’s no evidence that usual doses harm babies through breastmilk. I was surprised to read that breast milk doesn’t send loads of extra iron to babies, so getting enough in your own diet still matters.
Working with Your Doctor
Some women skip supplements because they worry about putting too much into their bodies. A conversation with your doctor solves most of those worries in five minutes. They’ll pull up your blood results and suggest the right dose. Sometimes, they recommend a different iron salt or offer tips for cutting down side effects. Pay attention to energy, skin tone, and sleep—subtle clues something’s off. Keep up with routine checks, especially if you feel weak or breathless.
Building Better Habits Around Iron
Adding iron-rich foods alongside supplements gives a stronger boost and might mean you can stop pills sooner. Lean meat, beans, lentils, and seeds make an easy start. A splash of orange juice helps, too—vitamin C boosts iron absorption. Watching out for coffee or tea at the same meal helps, since they slow things down.
Pregnancy and breastfeeding test strength and patience. No need to fight alone—ferrous fumarate has a long track record, but guidance from a professional shapes a plan that suits your health and your baby’s future.
Are there any interactions between Ferrous Fumarate and other medications?
Medicine Cabinets Are Crowded Spaces
Doctors hand out iron supplements like Ferrous Fumarate to help people who lack iron, usually due to anemia. It sounds simple—take a tablet, boost your blood. Life rarely plays out in straight lines, especially where medicine is concerned. Medicine cabinets stack up prescriptions: antibiotics, thyroid pills, stomach medicine, blood pressure tablets. In that mess, Ferrous Fumarate could clash with the other bottles, sometimes in ways that mess up treatment and leave the patient feeling frustrated or confused about why they aren’t getting better.
Common Interactions That Can Trip You Up
Calcium supplements and antacids show up in plenty of homes, especially for people dealing with bone issues or heartburn. They seem harmless but can block the body’s ability to soak up the iron from Ferrous Fumarate. Two weeks into taking both and a person might still feel wiped out, even though they're swallowing their iron faithfully every morning. The body just isn’t grabbing what it needs, wasting time and adding to worries.
Doctors set up tight schedules for some drugs like levothyroxine (for thyroid conditions) and tetracycline antibiotics. Ferrous Fumarate can tangle with these, making each less effective. Someone could take thyroid meds with their breakfast iron and wind up with low thyroid hormone levels, feeling foggy or tired. With antibiotics, the iron binds up the medication and less of it gets absorbed. Infections linger longer, and nobody wins.
Blood Thinners, Diabetes Drugs, and Surprise Twists
Warfarin, used to thin blood, brings its own list of food and drug rules. High doses of iron can sometimes introduce swings in lab values. Balancing the risks isn’t easy, and both doctors and patients need to pay attention. Iron also fights with metformin, a key diabetes medicine. Absorbing less metformin or less iron means unstable blood sugar numbers, or still facing symptoms of anemia after months taking both pills.
Stories from the Real World
On one pharmacy rotation, I remember an older man confused by his fatigue, thinking age was catching up with him. He was on a cocktail of antacids, blood pressure pills, diabetes medication, and Ferrous Fumarate. After a careful review and a chat with his doctor, his fatigue finally improved. He’d been taking everything at once in the morning. That meant his body didn’t pull enough iron out of the supplement, and the diabetes pill didn’t work as planned.
The Importance of Open Conversations and Checks
Nobody expects patients to memorize every possible interaction. It’s tough even for professionals. Keeping a current list of medications can help—on paper, in a notebook, or on a smartphone. Sharing that list with the pharmacist or doctor lets them spot problems and recommend practical changes, like separating doses by a few hours or switching the time of day. Some clinics now flag potential iron interactions in electronic records, but nothing replaces real conversation—patients need to speak up about all the pills, vitamins, and herbs being taken.
A Full Life, Not Just Full Cabinets
Taking Ferrous Fumarate isn’t just about following a prescription—it’s about understanding the mix, being open with health professionals, and keeping an eye on how you actually feel day to day. Juggling medications isn’t always easy, but with a few practical steps and a willingness to check in, it can get a lot safer—and folks can get back to living their lives, not just managing their medicine schedules.
What is Ferrous Fumarate used for?
Iron Shortage Hits Harder Than Most Think
Waking up already tired, feeling breathless climbing the stairs, getting headaches after light activity—low iron hits in subtle ways that can take a toll. Ferrous fumarate enters the picture for folks like this, offering a path back to feeling like themselves. Doctors see iron deficiency more often than many realize, especially in women, kids, and people who eat very little red meat. Where I live, blood donors often talk about being fatigued, only to discover their iron levels have bottomed out. The go-to fix often turns out to be a supplement, and ferrous fumarate stands out for both effectiveness and convenience.
A Powerful Weapon Against Anemia
Too little iron brings anemia—a condition that slows everyone down. Red blood cells need iron to carry oxygen. Without it, symptoms pile up: weakness, pale skin, brittle nails. Ferrous fumarate packs a punch because it delivers iron the body can use. Unlike some other iron salts, it tends to be gentler on the stomach. In the clinic, patients get this iron formulation to rebuild their supply, whether from diet shortfalls, pregnancy, or blood loss.
Iron for Pregnancy and Growth Spurts
Pregnancy drains iron at a shocking rate. As babies grow, they borrow from mom, who winds up short herself. Doctors don’t just recommend extra iron; they put women on ferrous fumarate specifically because it’s reliable and widely available. I noticed young kids and teens grab liquid or chewable versions for their own growth spurts. Pediatricians don’t hand this advice out lightly. They rely on years of research that show ferrous fumarate boosts hemoglobin and keeps complications at bay when used as directed.
Why Ferrous Fumarate Works Well
Plenty of iron minerals line pharmacy shelves, but not all get absorbed well. Some, like ferrous sulfate, trigger more stomach upset. Ferrous fumarate gives a decent amount of elemental iron—the kind the body uses right away. This matters because better absorption translates to faster improvement. In trials, people with iron deficiency saw clear gains in red blood cell counts. The World Health Organization and national health agencies include this supplement on lists of essential medicines for a reason.
Tackling the Stomach Side Effects
No iron supplement feels perfect. Nausea, constipation, and dark stools show up for some people. In family and community clinics, the trick often comes down to timing—taking it with food and sticking to a regular routine. Patients share tips with each other, like chasing an iron pill with orange juice for better absorption. Some even split doses through the day to keep side effects down. It’s far from a magic cure, but with a bit of guidance, ferrous fumarate brings most people back to health.
Making Iron Supplements More Accessible
Globally, low iron keeps millions from living their full lives. Community outreach, better nutrition education, and affordable supplements all matter. Over the years, health programs that hand out ferrous fumarate saw rates of anemia fall. One group delivered iron tablets to school-age girls, finding classroom focus and physical energy soared. Tackling the pills’ side effects with practical advice, plus clear language on why iron matters, brought lasting results where fancy solutions missed the mark.
How should I take Ferrous Fumarate?
Understanding Ferrous Fumarate
Iron matters, especially if your doctor says you need more. Ferrous fumarate is one of the forms of iron used to treat or prevent iron deficiency anemia. Some folks take it after surgery, some are prescribed it during pregnancy, and others just find their iron stores running low. It’s not uncommon; diets skip iron more often than you think.
How to Take Ferrous Fumarate for the Best Results
My family doctor always said, “Empty stomach if you can stand it.” That’s because your gut takes up iron better when there’s no food in the way. Food, especially things like tea, coffee, milk, and eggs, can slow how much iron your body grabs. Some days are rough on the stomach. If the pill sits heavy or makes you nauseated, have it with a small snack—just avoid dairy or high-calcium foods at that time.
Vitamin C gives a boost, so orange juice or a citrus fruit right before or after the dose helps. I worked shifts at a hospital pharmacy, and pharmacists swore by this combo: one iron pill and a glass of OJ. They saw lab results improve when patients stuck to that plan.
Staying Consistent, Not Perfect
Missing a dose isn’t the end of the world. If you remember later, just take it. Try not to double-up. Overlapping doses increase the odds you’ll feel queasy or get constipated. Iron takes time to build up in your system; a skipped day isn’t the end, but a pattern of missed doses slows recovery.
What Side Effects to Expect
Ferrous fumarate can be hard on the gut. Constipation ranks as the top complaint from people I talk to. Dark stools seem strange at first, but that’s normal. Diarrhea, cramps, or stomach pain sometimes crop up for others. If it gets severe, or you see blood in stool, check in with your doctor quickly.
Some folks get around constipation by eating high-fiber foods: whole grains, beans, veggies. Hydration helps more than you’d expect. If stomach upset keeps coming back, talk with your doctor. Sometimes a lower dose taken twice a day sits better than one full-strength pill. Liquid and chewable forms exist for people who can’t handle pills.
Why Sticking to Instructions Matters
Iron works best with consistency. Many people, especially pregnant women and young kids, come in low on iron. Anemia drags you down—tiredness, brain fog, pale skin, faster heartbeat. People working hard jobs, students burning late hours, and parents with busy homes all notice how much energy dips. Once iron pills become part of your routine, it might take weeks before you feel better. Blood tests track your progress. Ask for regular follow-ups if your symptoms linger.
The Bigger Picture
Most cases of iron deficiency have a fix: better diet, supplements, or treating a hidden medical issue. Make time for check-ups, eat foods like red meat, beans, leafy greens, and use supplements if a trusted health professional recommends them. Safe iron dosing matters. Keep pills away from kids, as a handful can cause serious harm. Trusted pharmacists and experienced doctors deal with iron questions every day; there’s no reason to guess or go it alone.
What are the side effects of Ferrous Fumarate?
Iron Is Essential, But Supplements Don’t Feel Light for Everyone
Growing up, my grandmother used to say that too much of anything gives a person trouble. Iron sits squarely in that camp. Doctors often recommend ferrous fumarate for people who struggle with iron deficiency. It’s affordable. Most pharmacies keep it in stock. But like anything that helps, it doesn’t always go down smoothly.
Common Side Effects People Deal With
Let’s cut straight to it. After starting ferrous fumarate, a lot of folks notice their stomach begins acting out. Constipation leads the list, along with stomach aches and occasional nausea. After a few days or weeks, toilet visits shift — not just in frequency, but in color. It's common to see stools turn darker. This change often sends people online searching for answers, unsure if things are going in the right direction.
I’ve seen some friends get so constipated they felt worse on the supplement than off. The iron in ferrous fumarate irritates the stomach lining and slows down gut movement. Drinking plenty of water helps, but rarely do those who start these pills avoid some cramping or bloating. Some report a strange metallic taste in the mouth right after swallowing it.
Less Common, More Serious Reactions
A smaller group notices symptoms that go beyond the stomach. Allergic reactions happen, though it’s not every day. Swelling of lips or throat, skin rashes, or trouble breathing means a call to the doctor is in order—fast. For those with health conditions like ulcers, Crohn’s disease, or other intestinal problems, ferrous fumarate might irritate their symptoms. One study in JAMA points to the risk of iron overload if people take it without monitoring blood tests. Iron builds up slowly in organs for some, especially people with hemochromatosis, even with what seems like an average dose.
Doctors Weigh In—Why Side Effects Matter
Iron deficiency doesn’t just steal energy; it hurts thinking, immune systems, and physical strength. Doctors face a puzzle: balance the need to raise iron levels, but avoid driving folks away with side effects. For those who can’t tolerate ferrous fumarate, nutritionists and primary care doctors look to tweak diets. Foods rich in vitamin C, such as citrus fruit or peppers, help the body grab more iron from beans, meat, and leafy greens.
Some clinics suggest slow-release iron, switching to liquid iron, or using alternatives like ferrous sulfate or gluconate. These swaps sometimes settle the gut better. Splitting doses to twice per day, instead of a big lump in the morning, limits pain for many. If things don't turn around, doctors investigate to see if the original diagnosis missed another cause.
Practical Tips—What Helps from Real-Life Experience
From what I’ve learned and seen, hydrating during the day and adding high-fiber foods like oatmeal or prunes helps beat back constipation. Taking iron with food might soften stomach pain for some, but this trick can shave off how much gets absorbed, so there’s a balance to strike. It’s awkward, but letting your doctor know about every side effect, even ones that seem silly, beats quitting on your own and risking worse anemia.
Iron isn’t the villain, but ferrous fumarate can feel rough for some. Better health comes from staying in touch with your medical team, not from toughing it out alone.
Can I take Ferrous Fumarate during pregnancy?
The Role of Iron in Pregnancy
Iron matters so much during pregnancy. Blood volume rises and the demand for oxygen shoots up as a baby develops. Without enough iron, moms can start feeling wiped out, dizzy, and run into bigger troubles like anemia. The American College of Obstetricians and Gynecologists points out that anemia affects up to half of pregnancies worldwide, and lack of iron is usually the reason. Developing babies depend on their mother’s iron to support their own blood and brain growth.
What is Ferrous Fumarate?
Ferrous fumarate is a common iron supplement, sold under a range of brand names in pharmacies. Doctors typically recommend it over other forms like ferrous sulfate because it’s gentle on the stomach for many women. A standard tablet usually provides 65 mg of elemental iron, which often lines up with what prenatal care calls for.
Choosing the Right Dose
Doctors don’t all write the same prescription for every pregnant woman. Some people need more iron than others. My own experience with prenatal care showed me that blood tests shape what the doctor advises. Some women are told to take daily iron with their prenatal vitamins. Others, especially when their blood count drops, might be told to add more iron to their day. Skipping iron or self-dosing can backfire and leave both baby and mom short on what they need.
Why Iron Deficiency Hits So Hard
Low iron often brings on profound tiredness that coffee can’t fix. Fainting spells and fast heartbeats aren’t just an inconvenience, they can create real risks for both mom and baby. Severe cases link to preterm birth, low birth weight, and lowered resistance to infection. Even brain development depends on it—the Centers for Disease Control and Prevention highlights how iron shortage can influence a child’s learning and memory later on.
Navigating Side Effects
Ferrous fumarate works well for most expectant mothers, but anyone who’s tried iron pills knows about the rough side, too. Nausea, constipation, and even a metallic taste often pop up. Doctors usually suggest taking iron with food if an empty stomach feels too harsh, but vitamin C-rich foods also help the body absorb iron better. I learned through trial and error that a glass of orange juice and iron together made a big difference.
Staying Safe With Supplements
Iron is essential, but too much can tip the balance. Large doses, especially when mixed with other supplements, can cause stomach upset or interfere with how other minerals get absorbed. The World Health Organization keeps the recommendation for pregnant women at around 30 to 60 mg per day unless a higher dose is prescribed after bloodwork. Iron overload can be dangerous, so checking in with a doctor before starting extra supplements protects both mom and baby.
Looking at Solutions and Next Steps
Pregnant women benefit from checking in early and often with their healthcare team. Iron levels change across each trimester, so regular blood tests help catch any dip before it causes issues. If iron pills cause too much trouble, liquid forms or different brands sometimes relieve symptoms. A healthy diet packed with beans, leafy greens, and lean meats fills in some gaps—real food never hurts.
Listening to best practices, following professional guidance, and paying attention to body signals create a safer and smoother pregnancy journey for both parents and baby.
Are there any interactions with other medications?
The Real-World Challenge of Mixing Medications
Taking more than one medication at a time seems pretty normal for most adults in the United States. A surprising number of people juggle several prescriptions each day, especially older folks who manage chronic diseases. This mix can create potential problems because drugs do not always work well together. Sometimes the effect of one medicine can get stronger or weaker just because another one is now in the mix. This is not just about prescription drugs—vitamins, supplements, and over-the-counter pain relievers all play a role.
What Happens When Medications Clash?
Drug interactions can shift the way the body processes certain medicines. For example, taking a blood thinner and aspirin at the same time without a doctor’s okay could lead to dangerous bleeding. Some antibiotics make birth control pills less effective, putting someone at risk of unplanned pregnancy. Even grapefruit can throw off how some cholesterol medicines work. I’ve seen friends scramble to manage blood sugar after adding a new cold medicine, only to learn their diabetes medication does not work as well when combined with certain decongestants.
Why Most People Miss the Signs
Most patients do not notice mild symptoms of drug interactions right away, or they blame them on something else—fatigue, a headache, a strange rash. People trust that what comes from a pharmacy shelf will work together just fine. Pharmacists and doctors have computer systems to flag obvious combinations, but nothing beats honest communication about every pill, patch, or supplement coming into the house. A lot of people fill prescriptions at more than one pharmacy, or pick up supplements at a grocery store, so their regular doctor may not know the full picture.
Staying Ahead of Possible Problems
Pharmacists have a huge role in keeping patients safe. I’ve gotten calls from pharmacists asking if my dad’s doctor really meant to prescribe two heart medicines with a known interaction. That watchful eye catches problems before they start. Patients can help by bringing written lists of medications to every medical appointment, and by speaking up if anything feels off shortly after starting a new treatment. Apps and online tools make it easier to keep track, but a handwritten list tucked into a wallet works too.
Science Backs Real Concerns
According to the Food and Drug Administration, over 50% of all side effects that send people to the emergency room stem from medication interactions. Polypharmacy—the routine use of five or more medicines—has become especially common in people over 65 due to multiple chronic conditions. Evidence shows that medication-related hospital visits drop when pharmacists and doctors review every person’s list at each visit. Research from the Mayo Clinic confirms that simple check-ins cut down on bleeding, confusion, and hospitalization caused by unwanted drug reactions.
Ways to Avoid Dangerous Interactions
Keeping every provider in the loop offers the best protection. People can take small steps like using the same pharmacy for all prescriptions, updating their medication lists often, and reading all drug information leaflets for new warnings. It gets tempting to take supplements just because they sound healthy, but doctors want to know about these too—the wrong mix can interfere or cause more side effects.
This topic hits close to home for many. Nobody wants their road to feeling better blocked by an unexpected medication clash. Open conversations and simple organization tools do more good than most realize, and could save a lot of unnecessary worry or harm along the way.
What is Ferrous Fumarate used for?
Iron Deficiency Can Slow Anyone Down
A few years back, a good friend confessed how tired she felt, even during short walks. Her doctor found her iron levels scraping the bottom. Ferrous fumarate, a type of iron supplement, showed up on her prescription. She didn’t realize how big a change that tiny tablet could spark.
Ferrous fumarate isn’t just another supplement people ignore at the store. Doctors often reach for it to battle iron deficiency anemia, which affects more than a billion people around the world. Many folks don’t realize how common low iron really is. Lack of it drags down energy, fogs up thinking, and in pregnant women, may even risk their baby’s health. Anyone who’s watched an active child suddenly lose steam or seen an older parent become pale and faint gets the picture: the body feels every shortage.
Iron By Any Other Name
Some iron pills leave a bad taste, cause cramps, or result in stubborn constipation. Ferrous fumarate offers a friendlier approach for many. It goes down easier and tends to upset stomachs less than other iron salts like ferrous sulfate. That’s crucial for someone who has to pop a tablet every single day, not just every once in a while.
A typical 325 mg ferrous fumarate pill packs about 106 mg of elemental iron, the form the human body actually absorbs. For folks fighting anemia, the goal is to give their system enough building blocks to make new red blood cells. Those cells carry oxygen everywhere, fueling muscles, sharp thinking, and even a sense of well-being.
People at Risk Can’t Afford to Ignore It
Women, especially during pregnancy and menstrual years, run a much higher risk of low iron. Children in rapid growth spurts and people on vegetarian or vegan diets may struggle too. Chronic health problems, like kidney disease or heavy bleeding, burn through iron stores much faster. Skipping the subject or brushing off fatigue with more coffee doesn’t solve the root problem. Multiple studies show that raising iron levels not only lifts energy, it also supports the immune system and brain function.
Doctors don’t just hand out iron tablets without a reason. Taking more than needed raises the risk of side effects and sometimes even poisoning, particularly in children. Blood work helps doctors decide who really needs iron and how much.
Small Habits Make a Difference
A lot of people don’t realize how iron gets absorbed. Vitamin C — say, a glass of orange juice with that tablet — can boost absorption. Tea and coffee, on the other hand, block it. Skipping iron-rich meals or relying only on supplements misses the point: food choices and timing play a big part.
Ferrous fumarate often provides a reliable boost for those who need it most. Regular check-ins with a healthcare provider help avoid both shortages and overload. It’s worth listening to your body and not ignoring signals like tiredness, paleness, or dizziness. Iron pills might not get glamorous headlines, but for folks who need them, they can change everything.
How should I take Ferrous Fumarate?
Why Ferrous Fumarate Matters
Iron keeps the body running strong—plenty of people know the tired feeling that comes with iron deficiency. Missing out on enough iron zaps your energy and drags down the immune system. Doctors often recommend ferrous fumarate to bump those levels up. This supplement finds its way into the routines of pregnant women, people with anemia, even athletes who have ramped up their training schedule. I’ve watched a family member struggle for months with the heavy, sluggish fog of iron deficiency. A simple iron supplement, taken the right way, offered real improvement.
Getting the Dose Right
The most common trouble people run into with iron isn’t the mineral itself, but the way it can upset the stomach. Nausea and constipation discourage folks from sticking with it, causing people to skip doses or abandon the bottle altogether. I learned from talking with pharmacists that taking ferrous fumarate with a small meal can soften the blow, even though empty stomach absorption stays best. A glass of orange juice—natural vitamin C—helps boost absorption, so that’s a real trick worth adding to the routine.
Simple Practices for Better Absorption
Milk, cheese, coffee, and tea in the same meal compete with iron—calcium and tannins block the gut from soaking up each dose. If the goal is to actually lift blood iron, spacing out ferrous fumarate from these foods makes the result far more predictable. My own habit became taking iron right before bed, well after dinner, teamed up with some vitamin C.
The Value of Consistency
Building up iron reserves in the body doesn’t happen overnight. Sticking to a schedule makes a big difference. The weeks pass by, and energy comes back bit by bit. Treating the supplement like a daily prescription, not a “take when you remember” habit, works better for everyone I know who has dealt with anemia in the long term. Skipped doses mean dragging energy out for months instead of weeks.
Watching Out for Side Effects
Ferrous fumarate sometimes changes the color of stool—it shifts dark, which can shock new users, but this is harmless. Noticing any real stomach pain, vomiting, or constipation that doesn’t let up? Reaching out to a healthcare provider early helps. Some people do best with a lower dose or a different type of iron entirely. There’s no shame in switching things up if the formula causes problems. Some supplements include stool softeners for this very reason.
Potential Solutions for Common Problems
Food diaries can help keep iron routines steady—recording what gets eaten and when pills go down makes it easier to spot patterns, both good and bad. Paying attention to how the body responds over time gives clues about what works best. Doctors can check bloodwork every few months to see if the dose matches the need. If stomach trouble keeps flaring up, talking to a healthcare provider about slow-release versions or different iron salts leads to fewer headaches.
The Bottom Line
Ferrous fumarate delivers real benefits but only if taken thoughtfully. The right timing, food pairings, and consistency turn a frustrating process into a success. People with personal experience or family history know that a sensitive stomach shouldn’t stop anyone from finally beating fatigue. Iron doesn’t work in isolation—habit, support, and a bit of trial and error solve most hurdles along the way.
What are the side effects of Ferrous Fumarate?
Iron Pills Aren’t Always Trouble-Free
Ferrous fumarate has become a household name for people dealing with low iron levels. Iron pills show up in medicine cabinets everywhere, especially among folks battling anemia. Doctors love this supplement for its ability to bring energy and strength back to tired bodies. Still, popping iron tablets each morning isn’t always smooth sailing, and many people find themselves wrestling with problems that these pills can trigger.
Facing Stomach Problems
Anyone who has ever started iron therapy probably knows the story. Your guts rebel not long after you take your dose. Constipation tops the chart of complaints. For some, this means days of discomfort, bloating, and the frustration of a system stuck in neutral. Loose stools or diarrhea can take over instead, so you never know which direction your stomach might turn. For plenty of iron users, daily habits change with pills—scanning labels to avoid anything that adds to the iron burden, staying close to bathrooms, taking pills with food, or trying to drink more water. The stubborn taste of iron can linger, too. I remember taking these pills as a teenager and dreading the metallic flavor and cramping that always followed. Doctors sometimes recommend splitting doses or switching supplements, but many just tough out these troubles.
Nausea and That ‘Off’ Feeling
Nausea hits hard for a lot of people. This side effect pushes some away from much-needed treatment. Queasiness may tag along after each dose, making meals seem less appetizing. People often quit their pills without telling anyone, which only prolongs the problem of low iron. Persistent heartburn or a burning feeling in the throat can come right behind nausea. This happens because ferrous fumarate can irritate the delicate lining inside the stomach and esophagus. Experts say taking these pills with food may soften the blow, but fats and fiber can also lower the absorption of the iron itself—a catch-22 for folks hunting for relief.
Black Stools Show Up
Stool often turns dark when people take iron pills. It’s a shock the first time, but black stool rarely means bleeding or anything dire—it simply signals that your body is processing extra iron. Once you know to expect it, the worry usually passes. Still, nobody tells you about this early on, and plenty of people feel anxious about what they see in the toilet.
Possible Skin Reactions and Rare Cases
Rashes, itchiness, or even hives sometimes show up. These aren’t the most common problems, but they can be serious if ignored. True allergic reactions to iron tablets remain rare, but it’s critical to contact a doctor if shortness of breath or swelling arrives. Children are at greatest risk for real harm from iron pills—just a handful of tablets can cause poisoning, so safe storage matters more than most people think.
Better Ways to Take Iron
Drinking lots of water, switching to slow-release versions, or trying a lower starting dose can soften the blow to your stomach. Some clinics even suggest taking pills every other day if your situation allows it, since newer research shows this might help absorption and comfort at the same time. Pairing ferrous fumarate with vitamin C—either in food or a supplement—boosts absorption naturally, though juice works better than acidic tablets for many stomachs. If nothing works, a doctor might suggest liquid iron or different forms altogether, like iron bisglycinate, which causes fewer gut complaints for some people.
Smart Monitoring Makes a Difference
Regular blood tests tell the true story about your iron status. By tracking your response, you catch problems before they grow. Every patient deserves a chance to feel better without trading one health problem for another. With honest conversations and a willingness to adjust the plan, reaching healthy iron levels doesn’t have to mean a constant battle with side effects.
Can I take Ferrous Fumarate during pregnancy?
Iron and Pregnancy: Why It Matters
Carrying a child pulls nutrients from everywhere. During my wife’s pregnancy, our doctor pointed out that iron runs low fast, and getting enough means a healthier mom and baby. With that, we looked into iron supplements, which can get confusing fast—ferrous sulfate, ferrous gluconate, and ferrous fumarate all in the drugstore aisle. Ferrous fumarate stood out since it packs more elemental iron per tablet than some other types, so doctors often reach for it when iron needs a serious boost.
The Science Behind the Recommendation
The Centers for Disease Control and Prevention (CDC) say pregnant women need about 27 mg of iron a day, almost double what’s needed before pregnancy. The World Health Organization flags iron-deficiency anemia as a wide-reaching problem in pregnancy, with serious risks: babies born too early, too small, or moms feeling wiped out, dizzy, or at risk for infection.
Ferrous fumarate is a common fix because it offers a high dose without taking handfuls of pills. Most tablets contain 210 mg of ferrous fumarate, giving about 68 mg of elemental iron. That fits right into what many obstetricians recommend for folks diagnosed with anemia during pregnancy—often, one tablet a day or as specifically prescribed.
What Doctors Ask Before Prescribing
No two pregnancies look the same. Some people tolerate iron pills well, others get stomach cramps or constipation, or the taste turns them off. Doctors check iron stores through blood work—ferritin, hemoglobin, hematocrit levels—before making recommendations. Folks with thalassemia or hemochromatosis might need something different, so self-diagnosing doesn’t cut it.
Mixing iron with food can ease stomach trouble but can block absorption. Dairy, calcium, and tea slow absorption, while vitamin C-rich fruits can help the body use iron better. I watched my wife swap her orange juice into breakfast on the days she remembered her pill, and that small adjustment worked wonders for her energy over time.
Risks and Common Sense Tips
Getting more iron than needed won’t give pregnancy a shortcut and could make things worse—nausea, dark stools, even more serious side effects with mega-doses. Always talk to a professional about supplements instead of testing on your own. Most prenatal vitamins have some iron, but not always enough to treat true anemia, so blindly doubling up can cause issues.
Consistent, small changes made the difference for us. Using a pill box, tying the iron dose to morning routines, and keeping a food diary with iron-rich meals—these little steps built lasting habits so deficiencies didn’t sneak up.
The Bottom Line
Ferrous fumarate isn’t the answer for everyone, but it gives clear benefits for many women fighting iron-deficiency anemia during pregnancy. With qualified medical guidance, the right dosing, and simple tweaks to daily habits, it makes a real dent in low energy and health risks.
Pregnancy already asks enough from families; supplement confusion shouldn’t add more stress. Solid advice, good nutrition, and mindful use of iron pills like ferrous fumarate can make this part of pregnancy a little easier to handle.
Are there any foods or medications that interact with Ferrous Fumarate?
Why Food and Medicine Pairings Matter
Ferrous fumarate shows up in countless prescriptions for people needing more iron. Doctors hand it out for anemia or just plain old low iron. For years, I watched relatives struggle with their iron pills, wondering why their body didn’t seem to soak them up. Turns out, some foods and medications get in the way without many people realizing it.
Common Foods Blocking Iron
Growing up, family meals always had big glasses of milk. Only later, I found out that calcium—plenty in milk and cheese—actually gets in a tug-of-war with iron absorption. Tannins in tea and coffee team up for the same result. Even though a cup of coffee offers comfort, it grabs hold of iron in your gut and drags it away before your body can use it. Studies from the NIH back this up, showing that tea or coffee with a meal can cut iron uptake by up to 60%.
So, I started to change my habits: orange juice in the morning and saving coffee for later. Vitamin C, especially in citrus fruits or strawberries, doesn’t just help with colds—it helps the body actually use the iron in ferrous fumarate. Vitamin C grabs the iron and keeps it safe until it gets absorbed. Mixing iron tablets with anything rich in vitamin C just makes good sense and has real science behind it.
Interactions With Medications
Pharmacies put warning stickers on iron bottles, but sometimes the message blurs. Common antacids like Tums or omeprazole can hurt iron absorption. Acid helps pull iron out of pills—and less acid means less iron in the bloodstream. Even antibiotics like tetracycline or ciprofloxacin fight for attention. If swallowed with ferrous fumarate, the two medicines tie each other up, and neither does its job well.
Many heart or thyroid medicines also react with iron supplements. For example, levothyroxine for thyroid issues or certain blood pressure drugs bind to iron, reducing both their powers. That’s not a rare event. According to the FDA, this sort of drug interaction sends thousands of people back to their doctor, wondering why nothing works right.
What Actually Helps?
Spacing out medicines with iron pills made a big difference for family members who struggled before. Taking ferrous fumarate two hours before or after other medications and calcium-rich foods kept things running smoother. The science lines up here—absorption nearly doubles in these cases. Keeping food diaries or pill organizers worked better than relying on memory.
Doctors and pharmacists have gotten better at highlighting these interactions, but people still miss the fine print. More clarity in prescription counseling—using plain language, repeat reminders, and follow-up calls—helps people actually benefit from their iron supplements. As a community, pressing for clearer directions and supporting public awareness campaigns gives everyone a better shot at healthy iron levels.
Diet and medicines can work together instead of against each other, but nobody benefits from a guessing game. Paying attention to the details on the bottle, asking follow-up questions at the pharmacy, and sticking with habits that help absorption set people up for better health and more energy.
| Names | |
| Preferred IUPAC name | (2E)-but-2-enedioic acid; iron(2+) |
| Other names |
Ferrous(II) fumarate Iron(II) fumarate Fumaric acid iron(II) salt |
| Pronunciation | /ˈfɛr.əs fjuːˈmæ.rət/ |
| Preferred IUPAC name | (2E)-but-2-enedioic acid; iron(2+) |
| Other names |
Fumaric acid, iron(II) salt Iron(II) fumarate Ferro fumarate Ferremia Hemocyte Fumasorb |
| Pronunciation | /ˈfɛr.əs fjuːˈmæ.rət/ |
| Identifiers | |
| CAS Number | 141-01-5 |
| Beilstein Reference | 1722996 |
| ChEBI | CHEBI:75879 |
| ChEMBL | CHEMBL1201563 |
| ChemSpider | 8758 |
| DrugBank | DB00103 |
| ECHA InfoCard | 100.014.330 |
| EC Number | EC 233-190-0 |
| Gmelin Reference | 84455 |
| KEGG | C00233 |
| MeSH | D023361 |
| PubChem CID | 25168 |
| RTECS number | LU8147000 |
| UNII | W1KS826B5T |
| UN number | UN3077 |
| CAS Number | 141-01-5 |
| Beilstein Reference | 3675953 |
| ChEBI | CHEBI:31544 |
| ChEMBL | CHEMBL1201562 |
| ChemSpider | 67644 |
| DrugBank | DB00103 |
| ECHA InfoCard | 31d6e7b5-47b4-4a4e-84b2-3750086511a9 |
| EC Number | 231-622-5 |
| Gmelin Reference | 130135 |
| KEGG | C18687 |
| MeSH | D000072243 |
| PubChem CID | 2723916 |
| RTECS number | QU7125000 |
| UNII | 7VY233R6Z5 |
| UN number | UN3077 |
| CompTox Dashboard (EPA) | DJ6H8AM34F |
| Properties | |
| Chemical formula | C4H2FeO4 |
| Molar mass | 169.93 g/mol |
| Appearance | Reddish-brown powder |
| Odor | Odorless |
| Density | Density: 2.435 g/cm³ |
| Solubility in water | Slightly soluble in water |
| log P | -2.70 |
| Vapor pressure | Negligible |
| Acidity (pKa) | 3.0 |
| Basicity (pKb) | 8.7 |
| Magnetic susceptibility (χ) | 'Paramagnetic (χ > 0)' |
| Viscosity | Viscous liquid |
| Dipole moment | 0.00 D |
| Chemical formula | C4H2FeO4 |
| Molar mass | 169.93 g/mol |
| Appearance | Reddish-brown powder |
| Odor | Odorless |
| Density | 2.435 g/cm³ |
| Solubility in water | Slightly soluble in water |
| log P | -1.23 |
| Vapor pressure | Negligible |
| Acidity (pKa) | 3.03 |
| Basicity (pKb) | Between 3.0 and 4.0 |
| Magnetic susceptibility (χ) | 'Paramagnetic (χ > 0)' |
| Viscosity | Viscous liquid |
| Dipole moment | Dipole moment of Ferrous Fumarate is 0 D |
| Thermochemistry | |
| Std molar entropy (S⦵298) | 186.4 J·mol⁻¹·K⁻¹ |
| Std enthalpy of formation (ΔfH⦵298) | -1517.4 kJ/mol |
| Std enthalpy of combustion (ΔcH⦵298) | -325.7 kJ·mol⁻¹ |
| Std molar entropy (S⦵298) | 252.7 J·mol⁻¹·K⁻¹ |
| Std enthalpy of formation (ΔfH⦵298) | -1648.6 kJ/mol |
| Std enthalpy of combustion (ΔcH⦵298) | -3122 kJ·mol⁻¹ |
| Pharmacology | |
| ATC code | B03AA02 |
| ATC code | B03AA02 |
| Hazards | |
| Main hazards | May be harmful if swallowed. Causes eye irritation. Causes skin irritation. May cause respiratory irritation. |
| GHS labelling | **"Warning; H302; P264; P270; P301+P312; P330"** |
| Pictograms | GHS07 |
| Signal word | Warning |
| Hazard statements | No hazard statements. |
| Precautionary statements | Keep out of reach of children. If swallowed, get medical help or contact a Poison Control Center right away. Store at room temperature away from moisture and heat. Do not use if you are allergic to any of the ingredients. |
| NFPA 704 (fire diamond) | 2-1-0 |
| Lethal dose or concentration | LD50 oral (rat): 1,130 mg/kg |
| LD50 (median dose) | LD50 (median dose): Oral-rat LD50: 830 mg/kg |
| NIOSH | SG |
| PEL (Permissible) | PEL: Not established |
| REL (Recommended) | 200 mg daily |
| IDLH (Immediate danger) | Not Listed |
| Main hazards | May cause irritation to the gastrointestinal tract if swallowed; may cause allergic reactions; harmful if large amounts are ingested. |
| GHS labelling | GHS07, GHS08 |
| Pictograms | GHS07 |
| Signal word | Warning |
| Hazard statements | Hazard statements: Not a hazardous substance or mixture according to Regulation (EC) No. 1272/2008. |
| Precautionary statements | Keep out of reach of children. If swallowed, get medical help or contact a Poison Control Center right away. |
| NFPA 704 (fire diamond) | 1-0-0-0 |
| Lethal dose or concentration | LD50 (oral, rat): 1,230 mg/kg |
| LD50 (median dose) | 830 mg/kg (rat, oral) |
| NIOSH | AB8575000 |
| PEL (Permissible) | PEL (Permissible Exposure Limit) for Ferrous Fumarate: Not established |
| REL (Recommended) | “Adult: 200 mg daily in divided doses” |
| IDLH (Immediate danger) | Not listed. |
| Related compounds | |
| Related compounds |
Fumaric acid Ferrous sulfate Ferrous gluconate Ferrous succinate Iron(II) chloride |
| Related compounds |
Iron(II) sulfate Ferrous gluconate Ferrous succinate Ferrous ascorbate Ferric chloride |