Ferric Pyrophosphate: More Than a Micronutrient
Historical Development
Ferric pyrophosphate goes back further than most people realize. In the early 20th century, scientists started hunting for ways to fight dietary iron deficiency. Old iron salts often tasted metallic, rusted quickly, and didn’t dissolve well in anything except acid. Chemists searching for a form that mixed more smoothly with common foods stumbled across ferric pyrophosphate—a compound that looks pretty plain in a textbook diagram but means a lot for public health. Hospitals noticed early attempts at iron fortification made food taste off, so researchers kept tweaking formulas until ferric pyrophosphate showed up as a hopeful alternative. Over decades, new ways of synthesizing it emerged, some through direct reaction of iron(III) salts with pyrophosphate under tightly controlled conditions. Each step in this history reflects a world trying to fix the quiet crisis of iron deficiency.
Product Overview
Ferric pyrophosphate doesn’t get much attention outside a chemistry classroom or food lab, but its reach extends everywhere iron deficiency threatens health—cereal, infant formulas, parenteral nutrition, pharmaceutical supplements. The compound itself is a yellow-white powder fine enough to blend with dry mixes or infuse directly into solutions. Unlike older iron sources, it tends not to clump or oxidize so much on the shelf, and it doesn’t carry a tell-tale metallic taste that would put people off their morning oats or a child off formula. For decades, brands searching for something that keeps flavor intact and iron available leaned toward ferric pyrophosphate.
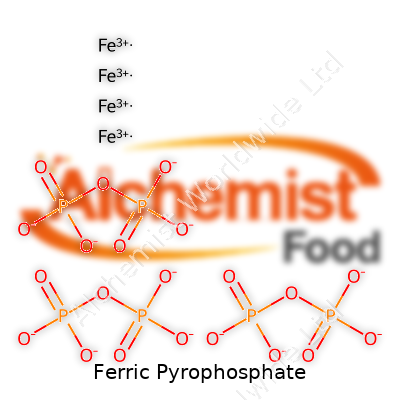
Physical & Chemical Properties
At room temperature, ferric pyrophosphate comes in a yellow to yellow-brown powder with a surprisingly mild smell. Its chemical formula—Fe4(P2O7)3—shows three pyrophosphate groups binding four iron atoms. The powder mixes poorly with water compared to other iron salts. Most forms won’t dissolve fully unless special mixing methods or binders help out, which can both help and hinder its use. This chemical stubbornness slows down its reactivity, making it less likely to damage the sensitive fats and vitamins found in many enriched foods. The iron in ferric pyrophosphate sits in the +3 oxidation state, not the easier-to-absorb +2, but with the right tweaks in the body or in a lab, it still serves its nutritional purpose.
Technical Specifications & Labeling
Manufacturers look at purity, particle size, solubility, and precise iron content. For food use, most authorities—like the EU’s EFSA or the US FDA—mandate food-grade purity above 95%, with iron content usually topping 25%. Particle sizes can range widely; smaller particles dissolve a bit better in some solutions, making them more useful in certain foods. The label on finished products using ferric pyrophosphate must disclose it as a source of iron and meet local and national health regulations on both iron quantity and safety, especially in infant nutrition or supplements. Besides “ferric pyrophosphate,” you might spot the ingredient list calling it “iron(III) pyrophosphate” or E379 in Europe.
Preparation Method
I’ve watched bench chemists make ferric pyrophosphate using two main approaches. The first involves mixing ferric chloride with a salt of pyrophosphate, usually disodium or tetrasodium pyrophosphate, in an aqueous solution. Stirring and heating push the formation of a light yellow precipitate—a raw compound ready for filtering and drying. The second method goes through a solid-state reaction using iron oxide and pyrophosphate salts at high temperatures, good for large-scale batch work. Both approaches demand tightly controlled pH and clean equipment to keep other metals and anions out. The product needs careful drying to avoid clumping or breaking down into less stable forms. It’s not flashy work, but precise handling at this stage makes all the difference for quality and safety.
Chemical Reactions & Modifications
In the lab, ferric pyrophosphate behaves with a stubborn sense of stability thanks to pyrophosphate’s grip on iron. Under acidic conditions—like what happens in the stomach—these groups break down, freeing the iron for absorption. In food applications, scientists sometimes coat ferric pyrophosphate particles with emulsifiers or special polymers, slowing unwanted reactions or masking off-notes. Some formulations boost absorption by combining it with enzyme-active compounds or mixing in tiny amounts of vitamin C, which can tip more iron into its bioavailable +2 state. Researchers have developed nano-sized ferric pyrophosphate dispersions for intravenous nutrition, using modifiers or chelators to keep the particles suspended, stable, and ready for direct entry into the bloodstream. Each innovation tries to maximize safety and usability without sacrificing quality.
Synonyms & Product Names
On shelves and datasheets, ferric pyrophosphate pops up under a handful of names. Besides its IUPAC favorite, “Iron(III) pyrophosphate,” it’s listed as E379 when used as a food additive. Some supplement brands just say “pyrophosphate iron” or “FePP” shorthand, especially in clinical nutrition products. Pharmaceutical suppliers may list CAS numbers 10058-44-3 or 1332-96-7 to avoid confusion with related forms. Major chemical producers give it proprietary names, but the real stuff in the bag stays the same—a mildly yellow fine powder, high in iron and often sealed in moisture-proof packaging.
Safety & Operational Standards
Safety teams treat ferric pyrophosphate as relatively low hazard for handling but keep an eye on dust exposure. The fine powder irritates if inhaled or gets in the eyes, so workers suit up with masks and tight-fitting goggles and monitor the workspace for airborne particles. Most regulatory agencies keep daily iron intake from supplements under close limits—40 mg of iron per day for most adults, with stricter numbers for children or those with pre-existing conditions. Storage practices call for cool, dry rooms away from acids and moisture, since exposure can break down the product or raise the risk of unwanted chemical reactions. Shipping follows strict labeling for traceability and transport safety, and recalls get launched fast if impurities sneak into a batch. On the user side, consumers are told to avoid doubling up on iron-fortified foods or supplements to dodge iron overload.
Application Area
You’ll find ferric pyrophosphate’s fingerprints in clinical nutrition, everyday foods, and even medical devices. Nutritionists choose it for orange juice, bread, baby cereal, and meal replacements—partly for its gentle flavor, partly for its relatively stable shelf life. Hospitals reach for it as part of parenteral (IV) nutrition solutions, especially when patients can’t eat by mouth or need careful iron dosing. Powdered supplements aimed at global nutrition use it to fortify children’s snacks or treat widespread anemia where absorption needs to happen with the least possible side effects. That wide net—from supermarket shelf to pediatric ward—explains its real-world importance.
Research & Development
Research on ferric pyrophosphate never quite slows down. One big push focuses on how to make iron more bioavailable: a fair amount of dietary iron in ferric pyrophosphate passes through unabsorbed without help, so labs experiment with nanoparticle forms, enzyme mimics, or combined supplements. Food scientists spend time figuring out how to keep color and taste unchanged at lower costs, studying coatings or binding agents. Clinical work explores new formulations for iron-deficiency anemia in chronic kidney disease, where speed and reliability count for a lot. Public health agencies keep field-testing fortified food programs with ferric pyrophosphate in regions hardest hit by anemia—Africa, Southeast Asia, and parts of South America. Crowdsourced data from NGO-run feeding programs now help shape how future products get designed, closing the gap between academic work and daily meals.
Toxicity Research
Toxicologists keep ferric pyrophosphate under a careful microscope. All iron supplements toe a tight safety line: too little leaves children tired and adults anemic, too much loads the liver and damages organs. Ferric pyrophosphate, thanks to its low solubility, causes less irritation to the gut compared to some iron salts—a point in its favor for sensitive patients. Chronic toxicity remains rare when admins stick to prescribed doses. Researchers track blood iron markers, gastrointestinal side effects, and organ function in both animals and humans to catch long-term problems early. The compound stands clear in most chronic exposure studies when used at therapeutic doses, but product formulation teams never take these findings for granted—they adjust guidance and labeling as new toxicology results appear. Careful consumer education emphasizes not mixing multiple sources of iron and watching for the classic warning signs of overload, like abdominal pain or persistent fatigue.
Future Prospects
Looking ahead, ferric pyrophosphate has a wide field in front of it. Global nutritionists keep hunting for better, safer iron sources as more people shift to plant-based diets and regions battle iron deficiency. Researchers continue working on ways to enhance absorption with less risk for digestive upset—using biochemical chelators, more absorbable particle sizes, or next-generation delivery vehicles. Consumer preference also shapes the market: milder flavors, transparent labeling, and sustainable sourcing all drive the next wave of product improvements. As more countries mandate iron fortification in staple foods, the demand for affordable, easy-to-blend iron sources only grows. In my experience, each real-world problem chased by scientists and food developers pushes innovation just a bit further—as a result, ferric pyrophosphate stands ready to anchor nutrition solutions for decades to come.
What is Ferric Pyrophosphate used for?
Iron Deficiency and the Need for Solutions
Iron deficiency shows up everywhere—from busy city hospitals treating anemia to parents worried about their children’s diets. As someone who has seen the toll of low energy and poor focus in friends living with iron deficiency, I pay special attention to how food and medicine deliver the right nutrients. Ferric pyrophosphate finds its way into these solutions, quietly supporting health in places most people never notice.
Making Foods More Nutritious
Makers of breakfast cereals, nutritional shakes, and baby formula rely on ferric pyrophosphate for one key reason: iron, on its own, often tastes metallic and can even change the look and flavor of food. Ferric pyrophosphate doesn’t bring these problems. Products keep their flavor, and people still get the iron their bodies crave. Some countries face widespread iron deficiency, especially among pregnant women and children. Adding ferric pyrophosphate to everyday foods answers a problem that touches millions worldwide.
Helping in Medical Treatments
Hospitals see many patients who can’t absorb iron easily from food. Some struggle with chronic kidney disease or inflammatory bowel conditions. Doctors use ferric pyrophosphate in intravenous or dialysate solutions. It slips iron right into the bloodstream, sidestepping digestion issues. Decades of medical trials back up its safety. Iron supplements take many forms, but ferric pyrophosphate works well because it treats patients gently, with fewer side effects like stomach pain or nausea.
The Science Backing Ferric Pyrophosphate
This iron compound doesn’t just blend into food or medical products; it works because science shows it releases iron steadily. Ferric pyrophosphate stays stable—meaning it doesn’t clump, change color, or lose its punch when mixed into food powders or liquids. Research in journals like the American Journal of Clinical Nutrition has confirmed its ability to raise iron stores over time, supporting better mental and physical performance in children and adults alike.
Avoiding Taste and Appearance Problems
Kitchens at home and at food companies face a simple battle: keep foods looking and tasting how people expect, but sneak good nutrition inside. Things like white rice or delicate milk powders pick up off-colors and flavors when traditional iron salts get used. Ferric pyrophosphate lets manufacturers keep foods appealing. Kids finish their breakfast. Parents avoid the power struggles that come with “funny tasting” health foods.
Room to Improve Access
Ferric pyrophosphate solves many problems, but iron deficiency remains far too common. Governments and non-profits could help by subsidizing fortified foods, especially in low-income areas. Schools and clinics already play a part, handing out supplements and running awareness programs. More local production of iron-fortified staples might bring costs down and reach communities faster than imported products ever could. Companies can also share clear information about what’s inside their foods. People have a right to know if their breakfast bowl is quietly saving them from anemia.
Looking Toward Better Health
Nobody wants extra pills with breakfast. Ferric pyrophosphate gets to work quietly, letting people live their lives while steering them toward better health. Food scientists, pharmacists, and policy makers have a role in making sure more people get the benefits. As iron deficiency continues to sap energy from millions, real change depends on bringing science, ethics, and practical action together.
Is Ferric Pyrophosphate safe for human consumption?
What People Need to Know
Ferric pyrophosphate shows up on nutrition facts labels, mostly in products claiming to offer iron without the taste or color changes of traditional salts. Bakeries use it in flour, baby formula brands tout it as a gentle iron, and meal replacements call on it to meet dietary iron targets. Friends have asked if it’s really any safer than the regular iron tablets doctors hand out or if all these “hidden” food additives start a new problem.
Iron in the Diet: More Than Just a Buzzword
Iron sits right at the center of human health. Not enough over months often means tiredness and headaches, especially for kids and pregnant women. Ferric pyrophosphate offers a version of iron designed to mix easily in foods. Instead of a metallic taste or dark streaks in bread, this additive dissolves without anyone noticing. It seems less likely to cause stomach upset or metallic aftertaste compared to ferrous sulfate or gluconate. For kids hesitant to take any medicine, these benefits matter.
What Science Says
Tons of research has gone into ferric pyrophosphate. Food safety agencies, like the FDA in the US and EFSA in Europe, gave their approval after years of data. Studies looked at both short-term reactions and results over several months. Healthy people who eat foods fortified with ferric pyrophosphate show clear rises in iron stores—no higher risk of diarrhea, constipation, or stomach troubles than those taking normal supplements. Babies, pregnant women, and adults all saw safe outcomes in clinical trials. Absorption rates tend to run a bit lower compared to some other iron salts, but the difference doesn’t seem big enough to change public health results.
Possible Drawbacks and Misinformation
Concerns float around every food additive, especially with families who already try to avoid too many unpronounceable ingredients. Some websites suggest iron fortification could harm people with disorders like hereditary hemochromatosis, but doctors would never recommend routine iron products to someone who absorbs too much iron. Using ferric pyrophosphate isn’t about masking hidden metals in food. Instead, it offers a real solution for populations where anemia remains stubbornly high and iron pills often get tossed aside due to taste.
Finding a Path Forward
Putting fortificants in food works best when paired with clear labels and strong education. That approach helps families with special medical needs make smart decisions. If a person wants to stick with the old-school iron pills, or skip fortified food, nothing stands in their way. People have every right to push for more research and tighter regulations, but calls for outright bans miss the bigger picture. In countries with high anemia rates, access to palatable iron can turn the tables for children, teens, and pregnant mothers. My own relatives struggled to swallow ferrous sulfate tablets—the switch to iron-fortified cereal or drinks made a night-and-day difference.
Trust but Verify
People deserve honesty from the food industry and real options in the grocery aisle. Reading the latest studies and talking with registered dietitians can cut through the panic and set the record straight. Based on current evidence, ferric pyrophosphate stands as a helpful tool in the fight against iron deficiency, with a track record built on science and human experience—not just industry hype.
What is the dosage or recommended daily intake of Ferric Pyrophosphate?
Understanding Why Ferric Pyrophosphate Matters
Iron deficiencies show up in more places than just hospitals and clinics. Many people feel tired, struggle with focus, or catch infections easily, not realizing it could be something as basic as not getting enough iron. Ferric pyrophosphate often shows up in nutritional formulas and supplements aimed at filling the gap. The form matters since it affects how easily the body absorbs iron and avoids some of the common side-effects like constipation. I’ve seen this firsthand, working with individuals who found traditional iron pills tough on their system, but felt better when they switched to supplements containing ferric pyrophosphate.
Recommended Intake: Always a Moving Target
Adults usually need about 8 to 18 milligrams of elemental iron each day, leaning toward the higher side for women of childbearing age due to menstrual blood loss. Ferric pyrophosphate delivers its iron content a bit differently than other sources, with a typical supplement providing dose options between 10 milligrams up to 30 milligrams, depending on what the product is trying to address. For example, I’ve worked with parents of children with kidney disease who use ferric pyrophosphate in doses adjusted specifically by the doctor, often much lower than what a healthy adult might need, because chronic illnesses change the body’s requirements.
Why Sticking to Guidelines Matters
I once met a young athlete who self-prescribed extra iron, thinking more would boost performance. Instead, he landed in the ER with stomach pain from too much iron. That’s a wake-up call: sticking close to recommended doses matters, especially since the safe upper level for daily iron intake hovers around 45 milligrams for adults, according to the National Institutes of Health. Anything beyond that can bring headaches – literally and figuratively.
Absorption and Food: Getting the Most Out of It
Most people take ferric pyrophosphate with food, since it skips a lot of the stomach troubles old-school iron pills cause. Still, even the best iron source doesn’t help if calcium-rich foods crowd out absorption. Orange juice with your supplement, for example, gives vitamin C that helps uptake, while a glass of milk at the same time just slows things down. Navigating these small choices makes a big difference. I encourage folks to look at the full picture, not just the supplement label.
Who Needs a Different Approach
Pregnant women need up to 27 milligrams of iron daily, so guidelines around ferric pyrophosphate fit that reality. People living with chronic kidney disease get ferric pyrophosphate through prescribed dialysate solutions or customized supplements. Their needs, set by a specialist, often change over time. On the flip side, adult men and postmenopausal women actually need less, unless there’s an underlying condition.
Weighing Risks, Benefits, and Next Steps
Before grabbing any supplement, check with a healthcare provider and get bloodwork done. They’ll catch specifics like ferritin and transferrin levels, not just total iron, which points toward real need. Chasing the perfect dose blindly opens the door to trouble. Charting a path with regular check-ups and a bit of nutritional awareness sets people up for real health, not just quick fixes.
Are there any side effects or risks associated with Ferric Pyrophosphate?
Looking Beyond the Labels
Ferric pyrophosphate pops up a lot in the world of nutrition. Companies use it to fortify everything from baby formula and meal replacement shakes to some breakfast cereals. This iron salt helps boost iron intake, fighting off anemia in folks who might not get enough through regular meals. Sound like a win? Some folks do get tripped up by the idea of supplementing with any kind of iron—asking about the side effects makes sense.
Upset Stomachs and Digestive Complaints
From personal experience, iron supplements don’t always sit well. Nausea, stomach cramps, bloating, and even diarrhea sometimes show up for folks taking iron salts. Ferric pyrophosphate is said to cause fewer stomach troubles than ferrous sulfate or ferrous gluconate, yet it’s not always smooth sailing. A 2022 review in the journal Nutrients pointed out that about 10% of people on iron supplements report tummy troubles, regardless of the salt used. With ferric pyrophosphate, the risk comes down a notch but doesn’t vanish altogether. Drinking plenty of water and taking it with food seems to help in my case.
Allergies: A Rare Worry, But Real
Some iron sources come wrapped in additional coatings or blended with stabilizers. That opens the door to allergic reactions, though these tend to stay rare. Symptoms like itching, swelling of the lips or face, and trouble breathing call for quick action. Most folks never run into this, but anyone with a known sensitivity should check all product labels or consult with a medical professional. It’s not paranoia—just smart to listen to your own body and history.
Overdose and Iron Buildup
Extra iron might seem harmless, but the body isn’t great at getting rid of too much. Consuming a large amount puts organs under strain. Symptoms of iron poisoning kick in—vomiting, fits of stomach pain, sometimes confusion or even organ damage over time. For people with hemochromatosis or chronic illnesses that cause iron overload, extra caution becomes vital. The best way to catch rising iron levels lies with regular blood work. Speak up during routine visits about any supplements you’re adding.
Kid-Sized Doses and Special Circumstances
Babies and kids, in my experience as a parent, need special attention when supplements come into play. Ferric pyrophosphate does show up in a lot of formulas and kids’ cereals because of its milder flavor and ease of mixing. Still, pediatricians often suggest letting them test a new product for a day or two before offering more. Some children get mild constipation or darker stool—a harmless but sometimes startling effect. Always run dosage changes by a pro, since every child absorbs nutrients a little differently.
Balancing Benefits and Risks
Sometimes, a low-iron diet turns life upside down. Ferric pyrophosphate offers hope for those struggling to get enough iron. As with all supplements, good advice and a level-headed approach lead to better outcomes. Sticking close to the recommended daily amount matters. Anyone managing chronic conditions, fixed budgets, or variable diets can benefit from a mix of careful self-monitoring, honest talks with doctors, and reading credible health sources like the World Health Organization or the National Institutes of Health. It isn’t about overthinking or doubling up on pills, just common sense and a willingness to adjust as needed.
How is Ferric Pyrophosphate different from other iron supplements?
Understanding Ferric Pyrophosphate in Everyday Terms
Iron makes a big difference to how our bodies work. It keeps our energy steady and helps blood do its job. Walk into a pharmacy and the shelves are stacked with many choices—ferrous sulfate, ferrous gluconate, ferrous fumarate. Ferric pyrophosphate usually flies under the radar. So, what's the catch? This form of iron behaves differently in the body and carries some clear perks and quirks.
Less Grit, Fewer Stomach Issues
From my own experience and talking with friends, gut troubles often lead people to drop their iron tablets. Cramping and those unmistakable black stools can ruin anyone’s morning. With ferric pyrophosphate, stomach side effects step back. Instead of flooding the gut with concentrated iron ions, it drips iron in slowly since it dissolves at a gentler pace. This is especially helpful if you or your child struggles to keep standard pills down or if you’re managing long-term conditions that already stress digestion. A double-blind study published in the Journal of Nutrition found ferric pyrophosphate to be far easier on the stomach, especially in large-scale fortification projects.
Absorption: Not Just About Swallowing
Some folks worry that if it’s easier on the gut, it probably doesn’t work as well. Here, it gets interesting. Ferric pyrophosphate doesn’t carry the same punch per dose as ferrous salts, since it’s less readily absorbed in the intestines. Ferrous sulfate often tops the chart because the body grabs it quickly. Ferric pyrophosphate takes more steps for the gut to pull it in. It still raises iron levels, but progress feels steady instead of dramatic. In populations with steady dietary intake or where supplements are added to food and drink (like in hospital nutrition), this gentle curve is an advantage—boosts iron over time without spiking side effects.
Food Fortification and Practical Solutions
Kids avoiding greens, older folks with poor appetites, and patients with dietary restrictions all face low iron. Ferric pyrophosphate slips into table salt, rice, and baby cereal without leaving odd flavors. The World Health Organization and Global Alliance for Improved Nutrition recommend this form for mass fortification. Big school lunch programs use it for this reason—it keeps food looking and tasting right. Try adding ferrous sulfate to orange juice and you’ll taste the problem. Ferric pyrophosphate lets nutritionists reach far more people, especially in regions where hunger turns iron deficiency into a bigger threat.
Cost and Access Remain Challenges
On the flip side, it isn't always the cheapest option. Ferrous salts have cornered the market in both cost and sheer availability. Many low-income settings stick with what's familiar, even if the side effects make people quit before finishing their treatment course. Improving affordability means more than just producing cheaper powders; it involves scaling manufacturing and convincing governments and health agencies that the benefits outpace the cost.
Real-World Decisions
Choosing the right supplement often boils down to real-life details: what’s available, what’s tolerated, and what fits within a person’s daily routine. For folks who can’t handle standard iron pills or live with conditions like chronic kidney disease, ferric pyrophosphate is a lifeline. The rest of us may weigh cost or speed of effect, but it pays to know why one choice may work better than another. Trusted sources—dietitians, doctors, and public health groups—make a big difference in sorting through these questions. Iron may be iron, but how we get it can shape our health for years.
| Names | |
| Preferred IUPAC name | iron(3+) diphosphate |
| Other names |
Iron(III) pyrophosphate Iron pyrophosphate Ferric iron pyrophosphate Iron(3+) pyrophosphate |
| Pronunciation | /ˈfɛrɪk paɪroʊˈfɒsfeɪt/ |
| Preferred IUPAC name | Iron(3+) diphosphate |
| Other names |
Iron(III) pyrophosphate Ferric diphosphate Iron pyrophosphate Ferripyrophosphate |
| Pronunciation | /ˈfɛrɪk paɪ.roʊˈfɒs.feɪt/ |
| Identifiers | |
| CAS Number | 10058-44-3 |
| Beilstein Reference | 683177 |
| ChEBI | CHEBI:61157 |
| ChEMBL | CHEMBL1201602 |
| ChemSpider | 157355 |
| DrugBank | DB09150 |
| ECHA InfoCard | ECHA InfoCard: 100.014.276 |
| EC Number | 263-448-9 |
| Gmelin Reference | 7851 |
| KEGG | C18639 |
| MeSH | D010948 |
| PubChem CID | 24817494 |
| RTECS number | UY7870000 |
| UNII | YD1QC1SWFM |
| UN number | UN3077 |
| CAS Number | 10058-44-3 |
| Beilstein Reference | 7840871 |
| ChEBI | CHEBI:37114 |
| ChEMBL | CHEMBL2107734 |
| ChemSpider | 16152 |
| DrugBank | DB09517 |
| ECHA InfoCard | ECHA InfoCard: 100.030.009 |
| EC Number | 231-835-0 |
| Gmelin Reference | 87886 |
| KEGG | C18691 |
| MeSH | D010959 |
| PubChem CID | 24865717 |
| RTECS number | TH7750000 |
| UNII | V9ZB3E6D3D |
| UN number | UN3077 |
| CompTox Dashboard (EPA) | Ferric Pyrophosphate CompTox Dashboard (EPA) string: **DTXSID2032210** |
| Properties | |
| Chemical formula | Fe₄(P₂O₇)₃ |
| Molar mass | 745.218 g/mol |
| Appearance | Greyish white powder |
| Odor | Odorless |
| Density | 1.5 g/cm3 |
| Solubility in water | Insoluble in water |
| log P | -17.7 |
| Vapor pressure | Negligible |
| Acidity (pKa) | 10.2 |
| Basicity (pKb) | 8.7 |
| Magnetic susceptibility (χ) | -38.0e-6 cm³/mol |
| Dipole moment | 0 D |
| Chemical formula | Fe₄(P₂O₇)₃ |
| Molar mass | 746 g/mol |
| Appearance | Yellowish-orange to green powder |
| Odor | Odorless |
| Density | Density: 1.5 g/cm³ |
| Solubility in water | Insoluble in water |
| log P | -18.6 |
| Vapor pressure | Negligible |
| Acidity (pKa) | NA |
| Basicity (pKb) | 8.2 |
| Magnetic susceptibility (χ) | 1.18×10⁻⁶ cm³/mol |
| Dipole moment | 1.49 D |
| Thermochemistry | |
| Std molar entropy (S⦵298) | 265.0 J·mol⁻¹·K⁻¹ |
| Std enthalpy of formation (ΔfH⦵298) | -2676.0 kJ/mol |
| Std molar entropy (S⦵298) | 237.8 J·mol⁻¹·K⁻¹ |
| Std enthalpy of formation (ΔfH⦵298) | -2676 kJ/mol |
| Pharmacology | |
| ATC code | B03AB10 |
| ATC code | B03AB10 |
| Hazards | |
| Main hazards | Harmful if swallowed; may cause irritation to skin, eyes, and respiratory tract. |
| GHS labelling | GHS07, GHS08 |
| Pictograms | GHS07,GHS09 |
| Signal word | Warning |
| Hazard statements | H319: Causes serious eye irritation. |
| Precautionary statements | Keep container tightly closed. Store in a cool, dry place. Use with adequate ventilation. Avoid breathing dust. Avoid contact with eyes, skin, and clothing. Wash thoroughly after handling. |
| NFPA 704 (fire diamond) | 1-0-0 |
| Lethal dose or concentration | LD50 (oral, rat): > 5,000 mg/kg |
| LD50 (median dose) | > 6,000 mg/kg (rat, oral) |
| NIOSH | WF182 |
| PEL (Permissible) | Not established |
| REL (Recommended) | 21 mg Fe/day |
| IDLH (Immediate danger) | Not listed |
| Main hazards | May cause irritation to eyes, skin, and respiratory tract. |
| GHS labelling | GHS02, GHS07 |
| Pictograms | GHS07,GHS09 |
| Signal word | Warning |
| Hazard statements | No hazard statements. |
| Precautionary statements | P264, P270, P301+P312, P330, P501 |
| NFPA 704 (fire diamond) | 1-0-0 |
| Lethal dose or concentration | LD50 (oral, rat): > 5,000 mg/kg |
| LD50 (median dose) | LD50 (oral, rat): >5,000 mg/kg |
| NIOSH | TTK44770V0N |
| PEL (Permissible) | 15 mg/m³ |
| REL (Recommended) | 21 mg/kg |
| Related compounds | |
| Related compounds |
Iron(II) pyrophosphate Iron(III) phosphate Ferric orthophosphate Ferrous sulfate Ferric chloride |
| Related compounds |
Ferrous pyrophosphate Ferric phosphate Iron(II) phosphate Iron(III) oxide Ferric ammonium citrate |