Cysteamine Hydrochloride: Looking Beyond the Lab Bench
Historical Development
Cysteamine hydrochloride has walked a winding road from discovery to practical use. Early work with cysteamine started in the 1940s, when researchers spotted its ability to break disulfide bonds—key connections in proteins. It first generated buzz in the treatment of cystinosis, a rare metabolic disorder that causes cystine to clog up cells. Scientists at the time relied on careful clinical observation and trial-and-error dosing to figure out the role cysteamine could play. Landmark studies in the 1980s solidified its application as a therapy for nephropathic cystinosis, saving kids from kidney failure. The process brought together biochemistry pioneers, pediatricians, and families fighting rare diseases.
Product Overview
Cysteamine hydrochloride today comes as a white, crystalline powder with a sharp odor—some say it reminds them of rotten eggs, thanks to the sulfur group. Drugmakers manufacture it in forms for both oral and topical use. Capsules, tablets, and ointments show up in clinics and pharmacies in North America, Europe, and Asia. A few companies also sell cysteamine hydrochloride as a certified pharmaceutical ingredient, supporting hospital compounding or research projects. The quality standards reflect strict regulatory guidelines, given the product’s use in delicate cases like pediatric nephrology.
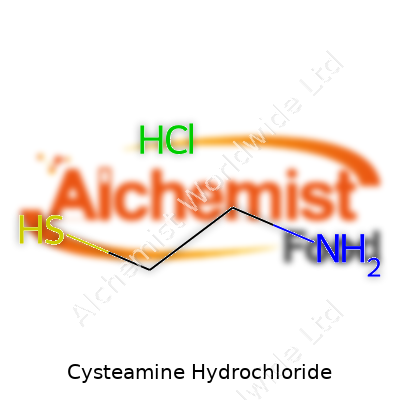
Physical & Chemical Properties
At room temperature, cysteamine hydrochloride remains stable, showing little tendency to degrade. Its melting point typically falls near 66-72°C, making it easy to handle in basic lab or manufacturing conditions. The compound’s chemical formula, C2H7NS·HCl, spells out its simple but reactive structure. With a strong affinity for water, it dissolves quickly and forms clear solutions—helpful for dosing accuracy. On the chemical side, the molecule boasts a primary amine and a thiol group. These two features give it both reducing power and the ability to interact with proteins through direct bonding. Not many biologically active compounds marry water solubility with such a reactive side chain.
Technical Specifications & Labeling
Good-quality cysteamine hydrochloride typically reaches a purity level above 98 percent. Pharmaceutical-grade products demand tight control over heavy metals, microbial counts, and related impurities. Labels must specify batch numbers, expiration dates, manufacturer information, and clear instructions for storage—usually a cool, dry place away from bright light. Package inserts provide dosing details and highlight the risks of accidental overdose, especially for patients with kidney or liver problems. In many countries, cysteamine hydrochloride lands on lists of controlled or prescription-only medicines, tightening oversight at every step from warehouse to bedside.
Preparation Method
Synthesis begins with cysteamine, which is typically generated by hydrolyzing cysteamine sulfonic acid or by the reduction of cystamine. Production lines blend the cysteamine base with hydrochloric acid under controlled temperatures to lock in the salt form without creating excess moisture. Filtration and drying steps follow, often under nitrogen to prevent oxidation of the thiol group. Scale-up to commercial production takes extra care to maintain purity, as trace contaminants can pass through into the finished medicine. The process walks a fine line: too much heat or acid, and breakdown products creep in; too little, and the yield drops.
Chemical Reactions & Modifications
Cysteamine hydrochloride’s free thiol group opens many doors in synthetic and industrial chemistry. It readily forms disulfides with other thiols, a property that underpins its role in breaking up protein aggregates in medical treatments. Many researchers use cysteamine as a starting material for more complex sulfur-containing drugs and biochemical probes. Alkylation or acetylation reactions help modify its reactivity, often to improve oral absorption or stability. These reactions occur under mild conditions and allow chemists to tailor cysteamine derivatives for experimental or clinical purposes.
Synonyms & Product Names
In the world of research and medicine, cysteamine hydrochloride wears several hats. It appears under names like mercaptoethylamine hydrochloride, β-mercaptoethylamine HCl, and 2-aminoethanethiol hydrochloride. Pharmaceutical brands include Cystagon and Procysbi for cystinosis, while compounding suppliers may list it by simple chemical name on catalogues. The synonymy sometimes causes confusion, underscoring the need for clear communication when ordering or prescribing across borders and specialties.
Safety & Operational Standards
Working with cysteamine hydrochloride calls for a healthy respect for safety guidelines. The compound can irritate eyes, skin, and respiratory passages on contact. Operators wear gloves, goggles, and lab coats during compounding. Spills need prompt cleanup, especially in confined spaces because of the strong odor and raunchy vapor. In bulk manufacturing, ventilation systems and local exhausts keep levels within occupational safety limits. Regulators like the FDA and EMA demand extensive documentation of every shipment, including provenance, test results, and chain-of-custody logs.
Application Area
The most important use for cysteamine hydrochloride remains as a therapy for nephropathic cystinosis. Children born with this genetic disorder face crystal buildup in their organs—without cysteamine, many would progress to kidney failure before reaching adolescence. Doctors also explore its potential in treating nonalcoholic fatty liver disease, neurodegenerative conditions, and certain types of cancer. On the cosmetic front, topical cysteamine earns attention for its ability to lighten skin affected by melasma or hyperpigmentation. Clinical trials still explore new territory—repurposing old drugs for diseases like Huntington’s and Parkinson’s draws interest from both academic teams and industry players.
Research & Development
After decades in rare disease clinics, cysteamine hydrochloride draws fresh scrutiny from scientific groups searching for low-cost therapies that tamper with cellular metabolism. Investigators map its routes into mitochondria, eyeing ways to enhance its tissue targeting. Studies probe combinatorial regimens, such as cysteamine plus antioxidants or anti-inflammatory agents, hoping to amplify its benefits or stretch out dosing intervals. Drug formulation teams experiment with sustained-release technologies to ease pill burden, especially for young kids who need round-the-clock therapy. Collaborations between pediatricians, pharmacologists, and families drive efforts to shape better-tolerated and more effective cysteamine products.
Toxicity Research
Long-term exposure studies reveal cysteamine hydrochloride’s double-edged sword: powerful therapeutic effects come with side effects. Nausea, vomiting, and strong body odor hit some patients hard, especially during the first weeks of treatment. In animals, high doses trigger gastrointestinal lesions and liver stress. Positive signals come from diligent monitoring—clinicians adjust doses and support hydration to reduce stomach upset, and new slow-release products tame peak concentration spikes. Researchers comb toxicology datasets looking for patterns that might signal rare risks or drug interactions. The emerging consensus emphasizes careful titration, especially in kids and anyone with preexisting digestive problems.
Future Prospects
Fresh enthusiasm surrounds cysteamine hydrochloride’s broader horizons. Ongoing studies test its power to limit oxidative stress in neurodegenerative disorders, as cheap oral therapies that slip across the blood-brain barrier remain rare. Dermatology researchers tweak dosing regimens to create over-the-counter creams gentle enough for everyday use, lowering barriers for people with stubborn dark patches. Teams in drug delivery focus on nanoparticle and liposomal forms, betting on improved efficacy and patient comfort. Worries about lingering side effects push the search for new derivatives that maintain biochemical advantages while sidestepping smell and stomach ache. Partnerships between academia and industry set the stage for new patents, but voices from rare disease advocacy warn against supply bottlenecks or sudden price hikes as demand spreads. In every conversation, patient outcomes set the tone: cysteamine must remain accessible, safe, and affordable for families counting on its continued availability.
What is Cysteamine Hydrochloride used for?
A Closer Look at Cysteamine Hydrochloride
Cysteamine hydrochloride often pops up in conversations among rare disease communities, but its role stretches beyond specialist clinics. For people with cystinosis—a hereditary disorder that builds up cystine in the body—cysteamine changes lives. Without this treatment, crystals form in organs, especially the kidneys, leading to pain, kidney failure, and sometimes even early death. Oral cysteamine started as a lifeline for these patients, helping to flush excess cystine from their bodies and slow down the damage.
Personal Connections in the Rare Disease Community
I once met a family whose child took cysteamine daily. Before the drug became available in an easy-to-take form, parents mashed up pills and measured out tiny doses on kitchen counters. Their kitchen looked more like a laboratory than a breakfast nook. Progress in pharmaceutical formulations made a huge difference for people like them. Because cystinosis affects only about 2,000 people worldwide, new drugs don’t show up quickly. It takes patients, doctors, and advocates pushing together to get the attention of drug companies. The experience of that family stuck with me—hearing them talk about how cysteamine kept their child out of the hospital put the power of a single medication in perspective.
Cysteamine's Role in Dermatology and Beyond
In recent years, cysteamine found new uses. It appeared in skin creams to target dark spots and skin conditions like melasma. Some doctors suggest it as an alternative to hydroquinone for people worried about long-term side effects. Studies have shown cysteamine cream can lighten dark patches just as well as more established treatments, often with fewer headaches over skin irritation or risk of ochronosis, a side effect of hydroquinone. For people who spent years searching for solutions to skin problems, this option provides a practical choice that didn’t exist for previous generations.
Safety, Accessibility, and the Struggle for Fair Pricing
Doctors who prescribe cysteamine watch out for side effects: bad breath, stomach upset, or, rarely, changes in blood cell counts. Most patients handle it well, but the drug’s specialized use sometimes drives the price up, putting it out of reach for people who need it most. Many families in the cystinosis community fight with insurance companies and see bills that stretch into the tens of thousands for a single prescription. This hits home—medicine isn’t just a scientific pursuit, but tied up with whether people can afford to stay healthy or even stay alive.
Affordable access remains a sore spot. Some generic versions entered the market, bringing prices down for a few but not for all. Charities and patient advocate groups work to fill in the cracks, helping families pay for what insurance won’t cover. In my experience, solutions pop up from the ground level more than from industry executives. Those living on the front lines—patients and caregivers—know the barriers intimately.
Looking Ahead for New Solutions
Research teams keep working on ways to make cysteamine easier to take and more effective. Improved drug versions aim to reduce side effects and help patients stick with treatment. Scientists are exploring more uses, from treating neurodegenerative conditions to combating certain forms of oxidative stress in cells. Still, the medication’s high cost and complicated approval process limit widespread adoption.
Cysteamine hydrochloride stands as an example of how a single medicine can shape the lives of rare disease patients and expand to benefit others. Its story highlights the everyday challenges of getting the right treatment at a fair price and reminds us of the real-world impact beyond the lab.
How should Cysteamine Hydrochloride be taken?
Taking the Pill, Not Just as Prescribed—But as Life Demands
Cysteamine Hydrochloride clocks in as an important medication for folks living with cystinosis. Doctors and pharmacists can say a lot about scheduled dosing, but people living with chronic treatments know there’s more to it. It’s not just about swallowing pills at the right time—it’s about threading meds into a life that’s already got routines, ups, setbacks, and busy meals.
Real Dosing Schedules Clash with Daily Life
Nobody loves alarms blaring at 2 a.m., but some people with cystinosis have dealt with this reality for years because missing doses means cystine crystals build up in their cells. From my work with families facing rare diseases, I’ve learned that skipping doses—even one—stirs up guilt, stress, and even a spiral of worry about long-term health risks. Every parent wants to help their children avoid late effects like kidney complications, and they know adherence is the biggest defense. Clinical research backs this up: stick with the dosing, and organ protection improves dramatically (National Institutes of Health data underscore this).
Empty Stomach, Not Empty Words
Doctors often push the empty stomach rule: take cysteamine at least 30 minutes before or 2 hours after meals. There’s science behind it. Food can block the medicine from being absorbed properly. Missing this window too often, and you risk losing the medicine’s power. It pays off to look at your meal schedule and see where those “empty” gaps fall naturally, maybe before breakfast, dinner, and bedtime. Some folks keep a log or set reminders—they get creative to protect their health.
Side Effects Aren’t Just “Part of the Deal”
Nausea, sulfur breath, and stomach upset aren’t just minor footnotes—these side effects push many to give up or skip doses. In my experience with support groups and clinical outreach, open, honest talks with the healthcare team shift the story. Instead of toughing it out, patients adjust with supportive meds, different formulations, or even a slow ramp-up in dose. Newer delayed-release formulas, with just two doses per day instead of four, can drop the burden a notch. Insurance, though, often raises hurdles, making the right medication dependent on coverage battles.
Integrating Family and Education
Children on cysteamine face obstacles their classmates don’t see. Absences pile up, and regular bathroom trips (from the medicine) sometimes single kids out. Families reach out to schools, crafting health plans with teachers, nurses, and classmates. It takes teamwork and honest conversation. Putting the child’s health needs at the forefront beats secrecy or silent suffering.
Quality of Life Gets a Voice
Sticking to prescribed cysteamine isn’t just a medical task—it’s tied to school, sleep, meals, and even friendships. The route of administration and timing affects everything from kidney status to how well someone sleeps each night. There’s nothing simple about chronic treatment, but open dialogue between patients, caregivers, doctors, and pharmacists raises adherence and lowers frustration.
Real change comes through support: reminder tools, school plans, easier formulations, and flexibility in care. Every dose counts, but every person counts more.
What are the common side effects of Cysteamine Hydrochloride?
Getting Straight to the Point
Cysteamine hydrochloride pops up in the treatment plans for folks battling cystinosis and sometimes in newer therapies for other rare conditions. You’ll recognize the name if you’ve spent time reading through prescription guides or talked to someone at the pharmacy counter. My time helping neighbors sift through their options taught me that every pill has a story—and usually, that story includes some side notes about what it does to the rest of your body.
What People Feel After Taking Cysteamine
Digestive issues lead the complaint chart here. Nausea likes to make an entrance early, and vomiting trails pretty close behind. Some people tell stories of a turning stomach after just a few doses. Diarrhea shows up more quietly but sticks around for some. From my own life, I watched a family friend power through a few weeks of upset, only to get relief after talking to their doctor about slower dose increases and meal timing. This matches the experience shared by many cystinosis support groups. GI symptoms—nausea, vomiting, diarrhea—affect over half of people starting cysteamine, according to published studies. Eating with each dose, instead of taking it on an empty stomach, helps.
Every doctor or pharmacist talks about the smell that comes along with this medicine. People mention a sudden whiff of rotten eggs, and it happens both in their breath and sometimes even their sweat. That sulfur scent can be tough to explain unless you’ve lived with it. I once helped a teenager manage the social stress of standing out this way, and it affected his confidence more than the doctors expected. The cause behind this is that cysteamine breaks down in the body to release sulfur compounds. It’s not dangerous, but it can feel embarrassing in public situations.
Dealing With Less Common Problems
Some complain about rashes or itchy skin. Skin problems happen in under 10% of people using cysteamine, according to clinical trial data. These rashes most often respond to antihistamines, but sometimes people need to switch to another medication. Headaches show up, too, along with sleepiness. My neighbor once called it “medicine fog”—hard to focus, just more tired than usual. These symptoms usually fade after a few weeks as the body adapts.
If the dose goes too high or ramps up too quickly, ulcers and mouth sores can develop. In rare cases, people develop joint pain or fever. For most, slow titration and regular check-ins with a care team help to head off the worst side effects. The best defense I’ve seen is frequent blood work and honest updates with doctors about what’s happening at home.
Staying Safe and Informed
Underpinning all this, the real harm comes when people keep quiet out of fear or embarrassment. Without direct conversations, side effects can fester into bigger trouble—missed doses, poor kidney health, and emotional strain. Taking cysteamine isn’t about pushing through; it’s about building a real relationship with care teams and finding a schedule that fits daily life. Pharmaceutical research highlights that open conversations keep both the medicine and patient on track.
If you or someone you love starts cysteamine, know that managing these side effects is possible. Clinics have experience here, and the solutions—dose adjustments, meal planning, odor control, support groups—made daily life better for many I’ve met. Facts and lived experience blend to help people keep their kidneys healthy without sacrificing their well-being.
Are there any drug interactions with Cysteamine Hydrochloride?
A Real-World Look at Cysteamine Hydrochloride
People sometimes rely on Cysteamine Hydrochloride for rare conditions, like cystinosis, where cystine builds up in cells and causes all sorts of problems. It helps clear out that extra cystine and improves kidney function, which often means a better, longer life for children who deal with this disorder. Taking a medicine every day, sometimes more than once, draws attention to what else might get mixed up in the process. Not everyone has had the same side effects or noticed problems, but I’ve seen several parents and patients wonder if their other prescriptions would tangle with Cysteamine.
What Science Tells Us About Drug Interactions
Cysteamine doesn’t usually share a lot of overlap with common medicines in a pharmacy cabinet. It works by breaking down cystine inside cells, and most over-the-counter meds don’t touch these pathways. Yet there’s no perfect medicine; every pill comes with a stack of information sheets for good reason. If someone is already taking drugs for seizures, the list narrows and the risk climbs. Medicines like phenytoin or phenobarbital can speed up how fast the liver breaks down cysteamine, leading to lower levels in the blood. When cysteamine dips, it may not work as well, and symptoms might creep back in.
Another common worry circles around metronidazole, an antibiotic that shows up for things like tooth infections or gut bugs. Used with cysteamine, the risk for side effects rises, especially if someone already has liver issues. This combo often leads to extra monitoring, and in some circumstances, doctors may pick a different antibiotic.
Levodopa—a go-to medication for Parkinson's disease—loses some punch when cysteamine enters the picture. Patients relying on both need to discuss this with their neurologist; dose adjustments or alternative therapies might work better. Iron supplements also play a part for people dealing with chronic kidney problems or anemia. Taking cysteamine with iron at the same time can get tricky because the absorption of one may block the other. Spacing them out by at least two hours keeps the supplements working properly.
The Human Side of Managing Interactions
Parents and patients who juggle multiple meds often develop a sixth sense about their routines. Maybe it comes from daily pill counting or learning to read every fine print insert before tossing the empty box. Missing an interaction isn’t just a technical mistake—it can land you or your child in the hospital. Even so, not every doctor or pharmacist spots rare conflicts, especially with less common drugs like cysteamine. My own conversations with specialists always end with the same request: “Are you on anything new?”
The best approach draws on solid relationships with healthcare professionals. Bring a full list of medications—prescriptions, vitamins, supplements—to each checkup. Pharmacies now use digital tools to detect conflicts, catching issues that used to slip through. If side effects show up, writing down symptoms and timing helps everyone connect the dots more quickly. Most problems have a simple solution, whether it’s shifting doses, adding extra blood tests, or swapping out a medicine.
Staying Safe and Informed
Cysteamine Hydrochloride can make a real difference for people with cystinosis and other rare diseases, but overlooking a drug interaction turns a good thing into a risky one. Reliable sources like the FDA, respected medical journals, and patient advocacy groups all highlight the importance of reviewing new prescriptions. At the end of the day, a quick phone call to a doctor or pharmacist could skip weeks of worry. Staying connected, asking questions, and watching for changes keep this medicine working for those who need it most.
Can Cysteamine Hydrochloride be used during pregnancy or breastfeeding?
Understanding Cysteamine Hydrochloride
Cysteamine Hydrochloride comes into conversation most in folks managing cystinosis, a rare genetic disorder. Over time, I’ve talked with parents and adults who navigate this medical journey every day. They rely on medications like this to manage symptoms, protect their kidneys, and keep life on a more even keel. But any medication can raise tough questions once parenthood, pregnancy, or breastfeeding come into play.
What's Known About Safety in Pregnancy
You look up the information on Cysteamine Hydrochloride, and you’ll see caution flags. Animal studies have shown risk to developing babies—from skeletal issues to miscarriages—when exposed to high doses. No one wants to be the test case here, and so far, there are no strong, long-term human studies examining what happens if a pregnant woman takes it. Regulatory authorities, including the FDA, flag it in Category C: only use it if the possible benefit justifies the possible risk to the unborn child.
Anyone facing this situation deserves clear information. Sometimes, stopping treatment brings on bigger problems. Cystinosis doesn’t take a break for pregnancy. Skipping medication could trigger organ damage or speed up decline, putting both parent and baby at risk. Talking through the balance of risks and benefits with a doctor who knows this medication well is key. Sometimes, specialists loop in OB-GYNs, nephrologists, and pediatric experts to personalize the approach.
Breastfeeding and Medication Transfer
After birth, the same questions pop up. Can you take Cysteamine Hydrochloride while feeding an infant? Small molecules often pass into breast milk, but data on exactly how much reaches a nursing baby are sparse. Some reports suggest Cysteamine could show up in milk, but the story stops there—long-term effects have not been closely studied in infants.
Mothers I’ve met often agonize over this choice. For rare conditions like cystinosis, peer support groups become lifelines. They share real-world experiences about balancing disease treatment and the wish to breastfeed. Guidance from medical teams often tips toward caution. If the only treatment for cystinosis is Cysteamine and pausing the drug brings risk, the conversation turns to alternatives, like switching to formula or using pumped milk from before medication resumption.
Facts Support Informed Decisions
The science never moves as fast as families wish. Food and Drug Administration records, combined with guidelines from groups like the American Academy of Pediatrics, keep pushing for more research. Right now, evidence supports the idea that women should only take Cysteamine Hydrochloride during pregnancy or breastfeeding if there’s no safer way to manage their condition—and if not treating the disease brings worse outcomes for mother and child.
As a father who watched my own partner make tough calls about medication, I know the peace that comes from a thorough talk with healthcare professionals. Bringing concerns, asking what’s new in the research, and checking what other options exist matter just as much as the label warnings. For rare diseases like cystinosis, the path forward will always lean on expert advice, open dialogue, and careful attention to emerging evidence. Those conversations can turn fear into something more like hope.
| Names | |
| Preferred IUPAC name | 2-aminoethane-1-thiol hydrochloride |
| Other names |
Cystamine 2-Aminoethanethiol hydrochloride Mercaptoethylamine hydrochloride |
| Pronunciation | /saɪˈstiː.ə.miːn haɪˈdrɒ.kləˌraɪd/ |
| Preferred IUPAC name | 2-aminoethane-1-thiol;hydrochloride |
| Other names |
Cystamine dihydrochloride Cystagon Cystadrops Cystaran |
| Pronunciation | /saɪsˈtiː.ə.miːn haɪˌdrɒ.kləˈraɪd/ |
| Identifiers | |
| CAS Number | 156-57-0 |
| 3D model (JSmol) | `3D model (JSmol)` string for **Cysteamine Hydrochloride**: ``` Cl.CSCCN ``` |
| Beilstein Reference | 82764 |
| ChEBI | CHEBI:60917 |
| ChEMBL | CHEMBL1200819 |
| ChemSpider | 54657 |
| DrugBank | DB06153 |
| ECHA InfoCard | 100.025.404 |
| EC Number | 200-157-7 |
| Gmelin Reference | 1237364 |
| KEGG | D01830 |
| MeSH | D03AX01 |
| PubChem CID | 6436344 |
| RTECS number | KH8580000 |
| UNII | P50657WI0U |
| UN number | UN1789 |
| CompTox Dashboard (EPA) | DTXSID9050702 |
| CAS Number | 156-57-0 |
| Beilstein Reference | 505748 |
| ChEBI | CHEBI:59790 |
| ChEMBL | CHEMBL1200906 |
| ChemSpider | 62738 |
| DrugBank | DB06153 |
| ECHA InfoCard | 100.026.914 |
| EC Number | 200-157-7 |
| Gmelin Reference | 60859 |
| KEGG | C07261 |
| MeSH | D03AX04 |
| PubChem CID | CID_6137 |
| RTECS number | KH8580000 |
| UNII | M7S94Q73FY |
| UN number | UN1781 |
| CompTox Dashboard (EPA) | DTXSID7020180 |
| Properties | |
| Chemical formula | C2H8ClNS |
| Molar mass | 113.61 g/mol |
| Appearance | White crystalline powder |
| Odor | Odorless |
| Density | 1.3 g/cm3 |
| Solubility in water | Freely soluble in water |
| log P | -2.5 |
| Vapor pressure | Negligible |
| Acidity (pKa) | pKa = 8.2 |
| Basicity (pKb) | pKb ≈ 3.3 |
| Magnetic susceptibility (χ) | -44.0e-6 cm³/mol |
| Refractive index (nD) | 1.658 |
| Viscosity | Viscosity: 18 cP (25°C, 2% in water) |
| Dipole moment | 2.41 D |
| Chemical formula | C2H7NS·HCl |
| Molar mass | 77.59 g/mol |
| Appearance | White or almost white crystalline powder |
| Odor | Odorless |
| Density | 1.3 g/cm³ |
| Solubility in water | Very soluble in water |
| log P | -2.36 |
| Acidity (pKa) | 8.3 |
| Basicity (pKb) | 7.75 |
| Magnetic susceptibility (χ) | -51.0e-6 cm³/mol |
| Refractive index (nD) | 1.670 |
| Viscosity | Viscous liquid |
| Dipole moment | 10.07 D |
| Thermochemistry | |
| Std molar entropy (S⦵298) | 117.7 J·mol⁻¹·K⁻¹ |
| Std enthalpy of formation (ΔfH⦵298) | -237.2 kJ/mol |
| Std enthalpy of combustion (ΔcH⦵298) | -569.1 kJ/mol |
| Std molar entropy (S⦵298) | 120.6 J·mol⁻¹·K⁻¹ |
| Std enthalpy of formation (ΔfH⦵298) | -242.6 kJ/mol |
| Pharmacology | |
| ATC code | S01XA15 |
| ATC code | S01XA15 |
| Hazards | |
| Main hazards | Harmful if swallowed. Causes skin irritation. Causes serious eye irritation. May cause respiratory irritation. |
| GHS labelling | GHS02, GHS07 |
| Pictograms | GHS05,GHS07 |
| Signal word | Warning |
| Hazard statements | H302, H315, H319, H335 |
| Precautionary statements | P261, P264, P271, P273, P280, P301+P312, P302+P352, P304+P340, P305+P351+P338, P308+P311, P330, P362, P405, P501 |
| Flash point | 76 °C |
| Autoignition temperature | 232 °C |
| Lethal dose or concentration | LD50 Oral Rat 652 mg/kg |
| LD50 (median dose) | LD50 (median dose): Rat oral 960 mg/kg |
| NIOSH | T201 |
| PEL (Permissible) | PEL (Permissible Exposure Limit) of Cysteamine Hydrochloride: 1 ppm |
| REL (Recommended) | 200 mg daily |
| IDLH (Immediate danger) | 100 ppm |
| Main hazards | Harmful if swallowed or in contact with skin. Causes skin irritation. Causes serious eye irritation. |
| GHS labelling | GHS05, GHS07 |
| Pictograms | GHS05,GHS07 |
| Signal word | Warning |
| Hazard statements | Hazard statements: H302, H315, H319, H335 |
| Precautionary statements | P261, P264, P271, P272, P273, P280, P302+P352, P305+P351+P338, P310, P321, P330, P362+P364, P501 |
| Flash point | 70°C |
| Autoignition temperature | 232°C (450°F) |
| Lethal dose or concentration | LD50 oral rat 652 mg/kg |
| LD50 (median dose) | LD50 (median dose): Oral - rat: 801 mg/kg |
| NIOSH | DT6650000 |
| PEL (Permissible) | PEL: 1 ppm |
| REL (Recommended) | 60 mg daily |
| IDLH (Immediate danger) | 100 ppm |
| Related compounds | |
| Related compounds |
Cysteamine Cystamine Penicillamine Cysteine Methionine |
| Related compounds |
2-Mercaptoethylamine Cystamine Cystine Cysteine Thiourea |